Study Finds That Cardiovascular Disease (CVD) Risk Factors Such As Age, Smoking And Diabetes Increase Risk Of COVID-19 Mortality And Not Preexisting CVD Itself!
Source: COVID-19 News Oct 13, 2022 2 years, 6 months, 1 week, 4 days, 11 hours, 43 minutes ago
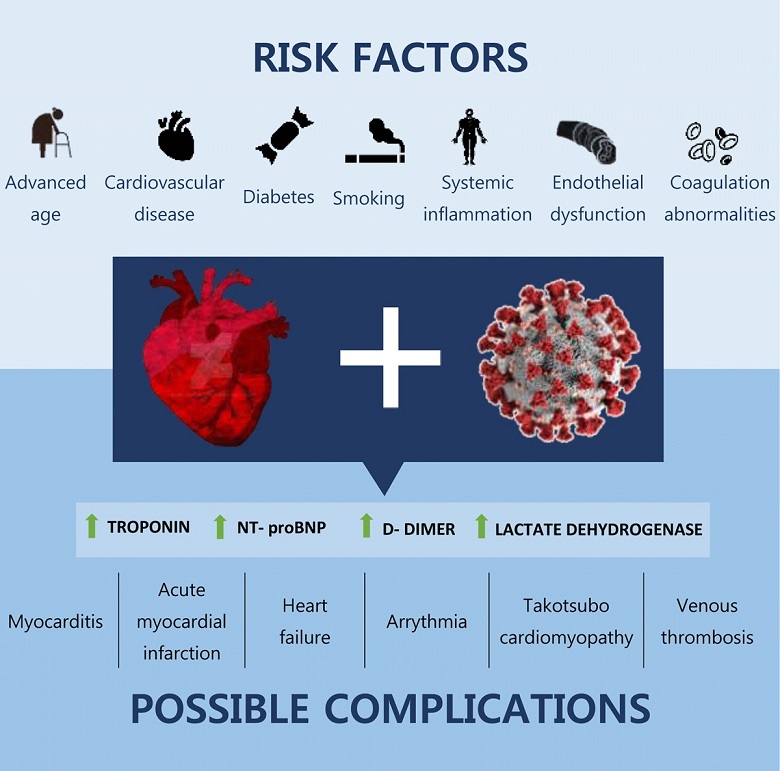
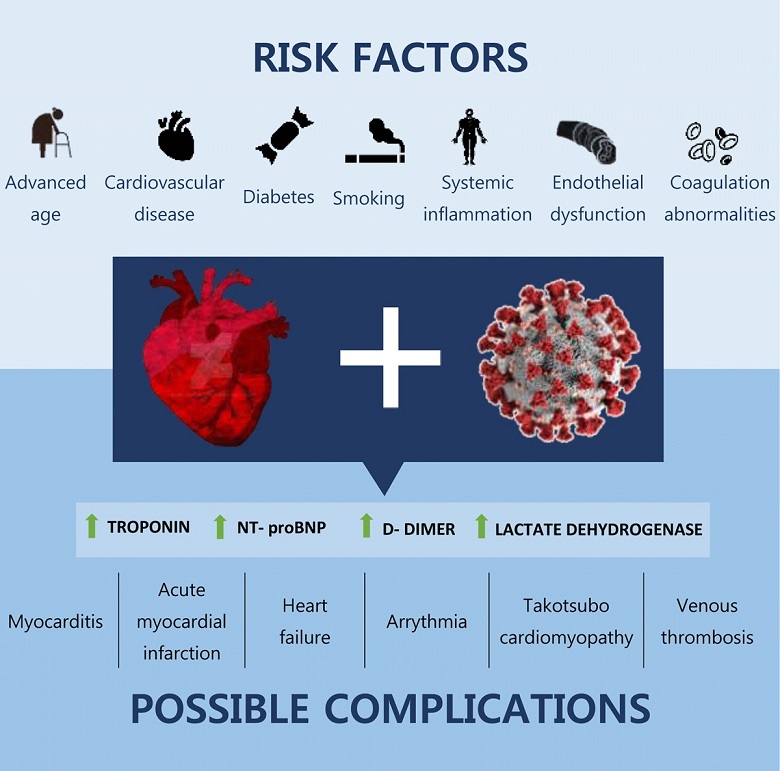
COVID-19 News: A new study by researchers from the University Of Michigan-USA has found that cardiovascular disease (CVD) risk factors such as age, smoking and diabetes increase the risk of COVID-19 mortality and not preexisting cardiovascular disease itself!
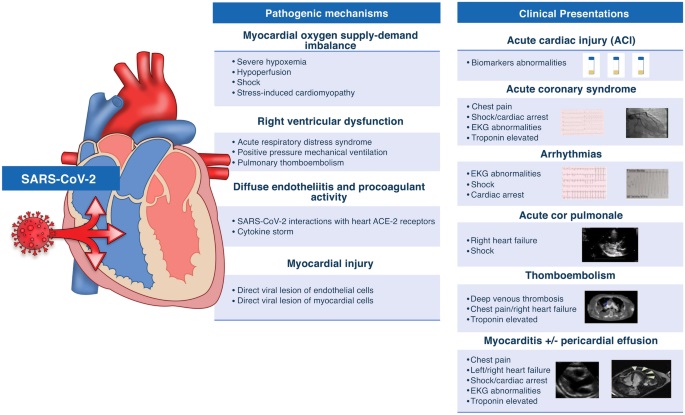
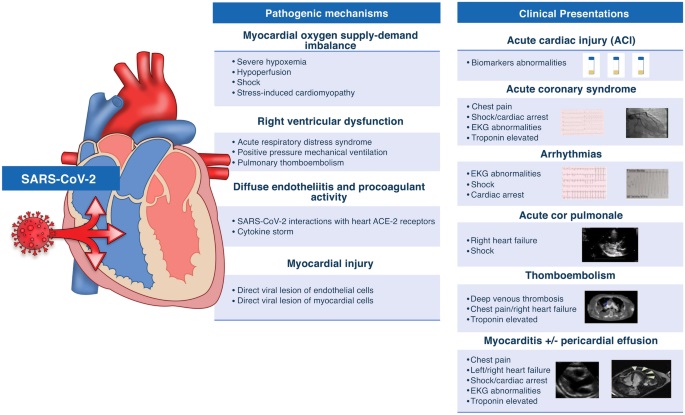
The study findings showed that the occurrence of myocardial injury, regardless of preexisting CVD, and its association with outcomes suggests it is likely due to multiorgan injury related to acute inflammation rather than exacerbation of preexisting CVD.
Currently there is a fallacy among the medical community that preexisting cardiovascular disease (CVD) was a risk factor for poor outcomes in patients with COVID-19. This has also been disseminated by various
COVID-19 News coverages in the past.
The study team sought to ascertain whether preexisting CVD is associated with in-hospital death and cardiovascular events in critically ill patients with COVID-19.
The research team used data from a multicenter cohort of adults with laboratory-confirmed COVID-19 admitted to intensive care units at 68 centers across the United States from March 1 to July 1, 2020. The primary exposure was CVD, defined as preexisting coronary artery disease, congestive heart failure, or atrial fibrillation/flutter.
Myocardial injury on intensive care unit admission defined as a troponin I or T level above the 99th percentile upper reference limit of normal was a secondary exposure. The primary outcome was 28-day in-hospital mortality. Secondary outcomes included cardiovascular events (cardiac arrest, new-onset arrhythmias, new-onset heart failure, myocarditis, pericarditis, or stroke) within 14 days.
In all, a total of 5133 patients (3231 male [62.9%]; mean age 61 years [SD, 15]), 1174 (22.9%) had preexisting CVD.
The study findings showed that a total of 1178 (34.6%) died, and 920 (17.9%) had a cardiovascular event.
Upon adjusting for age, sex, race, body mass index, history of smoking, and comorbidities, preexisting CVD was only associated with a 1.15 (95% CI, 0.98–1.34) higher odds of death.
Importantly, no independent association was observed between preexisting CVD and cardiovascular events.
However, myocardial injury on intensive care unit admission was associated with higher odds of death (adjusted odds ratio, 1.93 [95% CI, 1.61–2.31]) and cardiovascular events (adjusted odds ratio, 1.82 [95% CI, 1.47–2.24]), regardless of the presence of CVD.
The study findings showed that CVD risk factors, rather than CVD itself, were the major contributors to outcomes in critically ill patients with COVID-19. The occurrence of myocardial injury, regardless of CVD, and its association with outcomes suggests it is likely due to multiorgan injury related to acute inflammation rather than exacerbation of preexisting CVD.
The study findings were published in the peer reviewed journal: Circulation- Cardiovascular Quality and Outcomes.
https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.122.008942
&
amp;nbsp;
This is the first American nationwide study that found that risk factors for cardiovascular disease, such as age, smoking and diabetes and not preexisting heart disease are the main contributors to death and poor outcomes for critically ill COVID-19 patients.
 Existing Perceived Risk Factors For COVID-19 Severity And Mortality
Existing Perceived Risk Factors For COVID-19 Severity And Mortality
The study team analyzed outcomes for more than 5,100 patients admitted to intensive care units at 68 centers across the United States with severe COVID between March and June of 2020. Of those patients, 1,174 had either preexisting coronary artery disease, congestive heart failure or atrial fibrillation.
The study findings initially revealed that patients with cardiovascular disease had close to a 30% higher mortality rate than critically ill COVID patients without the preexisting condition.
But when adjusted for risk factors including age, sex, race, smoking and other factors such as diabetes, that relationship was no longer statistically significant.
Corresponding and senior author, Dr Salim Hayek, M.D., an Assistant Professor of Internal Medicine and Medical Director at University of Michigan Health Frankel Cardiovascular Center Clinics told Thailand Medical News, “Significantly, the fact that the association between cardiovascular disease and death was so heavily diminished when accounting for comorbidities suggests that cardiovascular risk factors rather than preexisting heart disease are the main contributors to in-hospital death in patients with severe COVID-19."
In the study, a total of 34.6% of patients died within 28 days and nearly 18% suffered a cardiovascular event, such as cardiac arrest or myocarditis.
The study findings showed that the association between such events and death did not differ between patients with and without preexisting heart disease.
Although cardiovascular disease is a common condition among patients who suffer severe COVID illness, given its prevalence among older adults and associated chronic inflammation, it is not a contributing factor to the outcome of the disease. In the study, age, obesity and diabetes were much stronger predictors of death due to COVID.
Importantly, regardless of whether a patient had preexisting heart disease, the study team found the presence of myocardial injury was associated with cardiovascular events and death.
It was found that myocardial injury was common among patients in the ICU, occurring in nearly half of patients who had heightened levels of troponin, a protein released when the heart muscle is damaged. Patients with the highest troponin measurements were nearly three times more likely to die than those without myocardial injury.
Dr Hayek added, "Although patients with severe COVID commonly had signs of cardiac injury, our study findings reinforce COVID-19 as a pulmonary disease with multi-organ injury related to systemic inflammation. The evidence of heart damage that we frequently see in patients with severe COVID-19 is more likely a reflection of the severity of the illness and the stress it imparts on all organs rather than the development of new complications or the exacerbation of preexisting heart disease."
Co-first author Alexi Vasbinder, Ph.D., R.N., a postdoctoral fellow in internal medicine at the University of Michigan stressed, “However, the study findings should not minimize the fact that patients with cardiovascular disease are still at risk for death due to COVID-19, as they have a high burden of risk factors for the disease, such as diabetes, hypertension and smoking.”
She added, "We are currently working on studies to further define groups of patients with COVID-19 at highest risk for severe outcomes, such as those with advanced heart failure or coronary artery disease.”
For the latest
COVID-19 News, keep on logging to Thailand
Medical News.