Nikhil Prasad Fact checked by:Thailand Medical News Team May 22, 2024 10 months, 1 week, 3 days, 17 hours, 52 minutes ago
Medical News: In recent years, the COVID-19 pandemic has left a significant impact on global health, introducing various complexities to medical science. A notable development is the rise in MDA5+ autoimmune lung disease, which has been linked to SARS-CoV-2, the virus responsible for COVID-19. This
Medical News report delves into the relationship between COVID-19 and the surge in MDA5+ autoimmune lung disease, exploring the immunopathological connections and the broader implications for healthcare.
 COVID-19 Is Causing Rise In MDA5+ Autoimmune Lung Disease
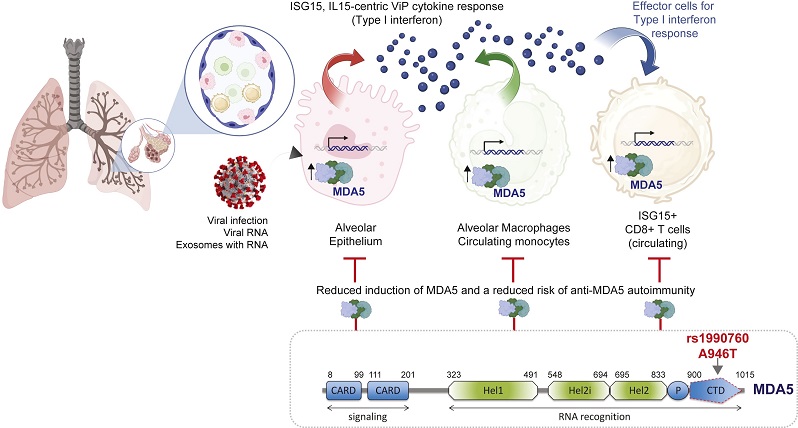
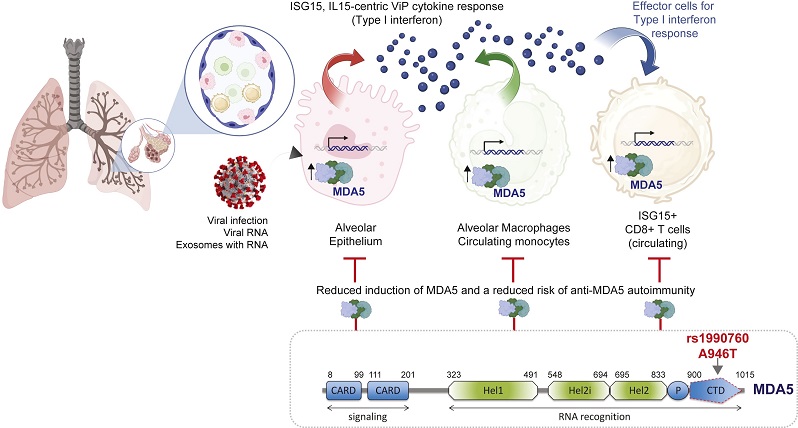
Schematic summarizes major conclusions and a proposed working model. A type 1-centric interferon response to the same could serve as pathophysiologic driver of autoimmune ILD involving more than one cell type. From left to right (Top): (i) In the alveolar pneumocytes of COVID-19 lungs, MDA5 is induced and is associated with type 1 interferon response, AT2 senescence and stem cell dysfunction. MDA5 is induced also in lung epithelial cells upon exposure to exosome vesicles from patients with acute infection. (ii) In the PBMCs of COVID-19 patients MDA5 is induced in infected samples, and its degree of induction positively and tightly correlates with an IL-15 centric type 1 interferon response. (iii) In the PBMCs of COVID-19 patients, there is a concomitant induction of a signature for anti-MDA5 autoimmune ILD expressed in ISG15+ CD8+ T cells. Bottom panel shows the impact of a protective genotype of the IFIH1 gene which inhibits a subset of patients from inducing MDA5 and thereby protects them from a surge of type 1 interferon storm.
Understanding MDA5+ Autoimmunity
-What is Dermatomyositis (DM)?
COVID-19 Is Causing Rise In MDA5+ Autoimmune Lung Disease
Schematic summarizes major conclusions and a proposed working model. A type 1-centric interferon response to the same could serve as pathophysiologic driver of autoimmune ILD involving more than one cell type. From left to right (Top): (i) In the alveolar pneumocytes of COVID-19 lungs, MDA5 is induced and is associated with type 1 interferon response, AT2 senescence and stem cell dysfunction. MDA5 is induced also in lung epithelial cells upon exposure to exosome vesicles from patients with acute infection. (ii) In the PBMCs of COVID-19 patients MDA5 is induced in infected samples, and its degree of induction positively and tightly correlates with an IL-15 centric type 1 interferon response. (iii) In the PBMCs of COVID-19 patients, there is a concomitant induction of a signature for anti-MDA5 autoimmune ILD expressed in ISG15+ CD8+ T cells. Bottom panel shows the impact of a protective genotype of the IFIH1 gene which inhibits a subset of patients from inducing MDA5 and thereby protects them from a surge of type 1 interferon storm.
Understanding MDA5+ Autoimmunity
-What is Dermatomyositis (DM)?
Dermatomyositis (DM) is an autoimmune disorder characterized by severe inflammation of the skin and muscles. It is also associated with interstitial lung disease (ILD), which leads to progressive pulmonary fibrosis. The first autoantibody linked to DM was anti-Mi-2, which targets the Mi-2 nuclear antigen. Over time, various myositis-specific and related autoantibodies (MSAs) have been identified, each associated with different clinical phenotypes.
-Clinically Amyopathic Dermatomyositis (CADM)
CADM is a variant of DM that significantly impacts the lungs, leading to progressive ILD. It is associated with the retinoic acid-inducible gene 1 (RIG-1)-like receptor family gene, IFIH1, which encodes the MDA5 protein. Unlike classical DM, CADM patients often present with skin-based symptoms such as tender palmar papules and skin ulceration, rather than the heliotropic rash typical of DM.
The Role of MDA5 in SARS-CoV-2 Infection
MDA5 is an RNA sensor and pattern recognition receptor that plays a crucial role in detecting SARS-CoV-2. Recent studies have shown that variants of the IFIH1 gene, which encodes MDA5, can confer protection against SARS-CoV-2 infections, leading to more favorable outcomes. This has highlighted the importance of unders
tanding the factors associated with MDA5+-related diseases, especially in the context of the COVID-19 pandemic.
Epidemiological Factors and Study Findings
A study conducted by researchers from the Leeds Teaching Hospitals NHS Trust and other institutions aimed to investigate the epidemiological factors causing the rise in MDA5+ cases during the COVID-19 pandemic. The study examined data from January 2018 to December 2022, noting a significant increase in MDA5+ cases following the second wave of COVID-19. In particular, the number of new MDA5+ cases rose from six between 2018 and 2019 to 60 between 2020 and 2022.
Clinical Characteristics and Outcomes
The study revealed that 42% of MDA5+ cases were associated with progressive ILD, with a third exhibiting aggressive ILD. Transcriptomic analyses indicated that the surge in MDA5 autoimmunity during COVID-19 was likely due to shared aberrant type 1-centric interferon (IFN) responses, distinct from idiopathic pulmonary fibrosis (IPF). These findings were consistent with global reports, suggesting a link between SARS-CoV-2 infection and MDA5+ autoimmunity.
Exploring the Mechanisms: Shared Immunopathology
Researchers utilized transcriptomic datasets to explore the shared mechanisms between MDA5-associated disease and COVID-19. They compared autoimmune lung disease, acute COVID-19 lung disease, and IPF to understand the origin of the MDA5+ DM outbreak. A model was developed linking severe anti-viral cytokine response with IFIH1 stimulation, leading to the unique immunophenotype associated with MSA-related progressive ILD.
Gene Expression Patterns
Gene expression studies highlighted the induction of the IFIH1 gene in various cell types during COVID-19, particularly in bronchoalveolar lavage fluid from COVID-19 patients. This induction was associated with an intense IL-15-centric type 1 IFN response, a hallmark of progressive ILD in systemic autoimmune rheumatic diseases. This connection suggests that the immune response to SARS-CoV-2 may trigger or exacerbate MDA5+ autoimmunity.
Implications and Future Directions
Proposed Term: MIP-C
The study proposes the term MDA5-autoimmunity with interstitial pneumonitis cotemporaneous with the COVID-19 pandemic (MIP-C) to describe this phenomenon. This term reflects the distinct epidemiology and clinical patterns observed during the pandemic compared to previously defined MDA5-related autoimmunity. The MIP-C phenotype has similarities to multisystem inflammatory syndrome in children (MIS-C), with many cases occurring without a confirmed history of COVID-19.
Vaccination and MDA5+ Disease
The study found that approximately 42% of new MDA5+ cases were not vaccinated before the onset of the disease, indicating that even mild or asymptomatic COVID-19 infection could trigger MDA5 autoimmunity. This raises questions about the potential role of vaccination in inducing such autoimmune responses. Further research is needed to understand the immunogenicity of SARS-CoV-2 vaccines and their interaction with MDA5.
Clinical Management and Future Research
Given the significant rise in MDA5+ cases during the COVID-19 pandemic, it is crucial to monitor and manage this condition effectively. The study highlights the importance of recognizing MIP-C as a distinct syndrome, which may require different therapeutic approaches compared to pre-pandemic MDA5+ disease. The findings also emphasize the need for multicenter studies across nations to validate these observations and better understand the global clinical burden of MIP-C.
Conclusion
The COVID-19 pandemic has introduced new challenges and insights into the field of autoimmune diseases, particularly MDA5+ autoimmunity. The surge in MDA5+ cases during the pandemic underscores the complex interplay between viral infections and autoimmune responses. Understanding the shared immunopathology between COVID-19 and MDA5+ autoimmunity is essential for developing effective diagnostic and therapeutic strategies. As we continue to navigate the aftermath of the pandemic, further research and collaboration will be critical in addressing the evolving landscape of autoimmune diseases.
The study findings were published in the peer reviewed journal: eBioMedicine.
https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(24)00171-3/fulltext
For more about MDA5+ Autoimmune Lung Disease, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/breaking-doctor-from-uc-san-diego-warns-of-new-covid-19-manifestations-such-as-dermatomyositis-muscular-pains-and-alerts-about-lung-fibrosis