Study Finds That SARS-CoV-2 Activates IRE1alpha-XBP1 Arm Of The Unfolded Protein Response And That Fluvoxamine Was Not Effective In COVID-19
Nikhil Prasad Fact checked by:Thailand Medical News Team Apr 21, 2024 1 year, 3 days, 19 hours, 23 minutes ago
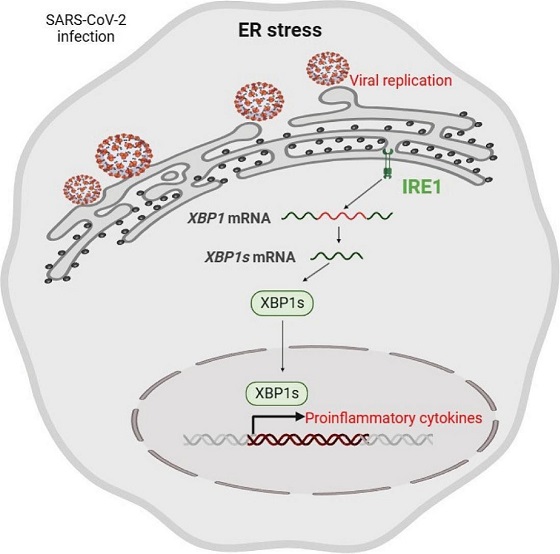
COVID-19 News: The ongoing COVID-19 pandemic caused by the SARS-CoV-2 virus has led to substantial global health challenges. One of the severe complications associated with SARS-CoV-2 infection is pneumonia, characterized by heightened inflammation reminiscent of a cytokine storm. This phenomenon, where an excessive production of cytokines occurs, is closely tied to the activation of the unfolded protein response (UPR). The UPR is a cellular pathway that responds to ER stress, a condition triggered by the accumulation of misfolded proteins in the endoplasmic reticulum (ER). The UPR consists of three branches regulated by sensors such as IRE1, PERK, and ATF6, which play crucial roles in maintaining cellular homeostasis.
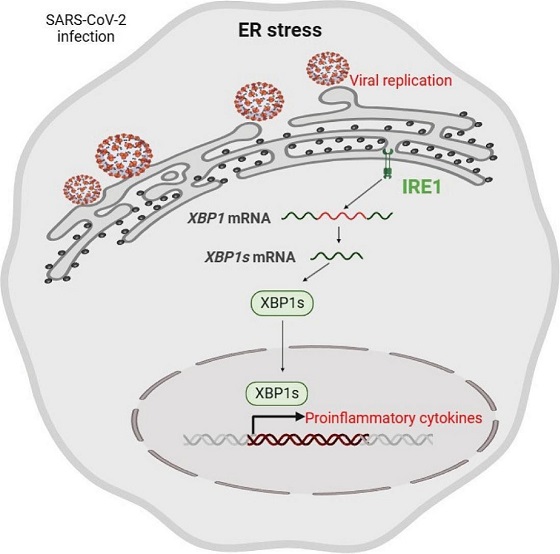 Graphical Abstract - SARS-CoV-2 Activates IRE1alpha-XBP1 Arm Of The Unfolded Protein Response
Research Objectives and Methodology
Graphical Abstract - SARS-CoV-2 Activates IRE1alpha-XBP1 Arm Of The Unfolded Protein Response
Research Objectives and Methodology
To delve deeper into the relationship between SARS-CoV-2 infection and the UPR, a collaborative study that is covered in this
COVID-19 News report, involving researchers from institutions including the Unidad de Excelencia Instituto de Biomedicina y Genética Molecular in Spain, the Icahn School of Medicine at Mount Sinai in the USA, and several universities in the UK was undertaken. The primary objectives were to investigate how SARS-CoV-2 activates specific arms of the UPR, its impact on proinflammatory cytokine production, the role of UPR in viral replication, and the potential therapeutic implications of these findings.
Findings from In Vivo and In Vitro Models
The study utilized both in vivo models, including mice and Syrian hamsters infected with SARS-CoV-2, and in vitro models using human lung epithelial cells. The results revealed a significant activation of the IRE1α-Xbp1 arm of the UPR in response to SARS-CoV-2 infection. This activation was closely associated with increased production of proinflammatory cytokines, highlighting the link between UPR and the inflammatory response observed in severe COVID-19 cases. Moreover, the researchers observed a dependency of viral replication on UPR-target proteins, particularly those associated with the IRE1α-XBP1 arm, in lung epithelial cells.
The Key findings were:
-SARS-CoV-2 infection of mice and Syrian hamsters activates the Ire1α-Xbp1 arm of UPR.
-SARS-CoV-2 leverages the Ire1α-Xbp1 arm for replication in lung epithelial cells.
-Ire1α-Xbp1 arm activity is associated with proinflammatory cytokine production.
-The IRE1α-XBP1 arm is activated by Spike proteins from different variants of concern.
Implications for Therapeutic Strategies
Understanding the molecular mechanisms by which SARS-CoV-2 hijacks cellular pathways like the UPR sheds light on potential therapeutic targets. While current treatments for severe COVID-19 focus on mitigating inflammation, such as the use of dexamethasone and
tocilizumab, exploring UPR modulation as a complementary approach gains significance.
The study also investigated the effects of fluvoxamine, a selective serotonin reuptake inhibitor (SSRI), on UPR activation and cytokine levels in infected mice. Although fluvoxamine showed a reduction in peripheral blood cytokines, its impact on viral replication was not significant, suggesting a complex interplay between UPR modulation and viral pathogenesis.
Unraveling the Role of Spike Proteins in UPR Activation
Another intriguing aspect of the research was the examination of Spike (S) proteins from different variants of concern (VOC) of SARS-CoV-2 and their ability to induce UPR activation. The findings revealed a consistent activation of the IRE1α-XBP1 arm by these Spike proteins, highlighting their role in promoting viral replication and cytokine expression. This underscores the importance of Spike proteins not only in viral entry but also in modulating host cellular responses, including the UPR.
Conclusion and Future Directions
In conclusion, the study provides valuable insights into the intricate interplay between SARS-CoV-2 infection and the unfolded protein response. The activation of the IRE1α-XBP1 arm of the UPR contributes significantly to the hyperinflammatory state observed in severe COVID-19 cases and enhances viral replication. Future research avenues could explore targeted therapies aimed at modulating specific branches of the UPR to attenuate both inflammation and viral propagation. Additionally, continued investigation into the role of viral proteins, such as Spike proteins, in UPR activation may unveil novel strategies for combating COVID-19 and related respiratory illnesses.
The study findings were published in the peer reviewed journal: Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.
https://www.sciencedirect.com/science/article/abs/pii/S0925443924001820
For the latest
COVID-19 News, keep on logging to Thailand Medical News.