Study shows human infections of H5N1 bird flu in America is far more than what is being officially reported
Nikhil Prasad Fact checked by:Thailand Medical News Team Aug 01, 2024 1 year, 4 months, 3 weeks, 2 days, 21 hours, 37 minutes ago
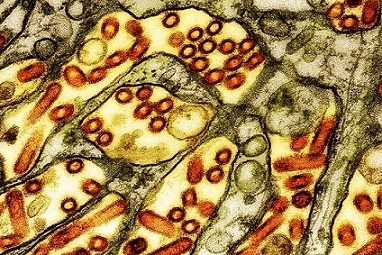
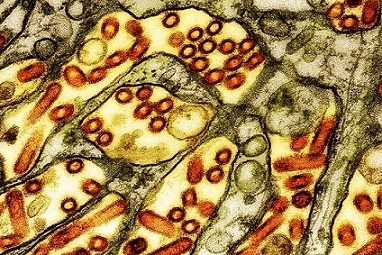
H5N1 News: H5N1 Bird flu, or avian influenza, has long been a threat to both animal and human health. The highly pathogenic avian influenza virus (HPAIV) H5N1 subtype is particularly concerning due to its potential to cause severe disease and its ability to spread across species. A recent investigation into the presence of H5N1 on dairy farms in Texas has revealed alarming findings about the virus's spread and its potential implications for public health.
 Human infections of H5N1 bird flu in America is far more than what
Human infections of H5N1 bird flu in America is far more than what
is being officially reported
The Undetected Threat
The Centers for Disease Control and Prevention (CDC) has raised concerns about the potential undetected spread of bird flu among farmworkers. Despite the lack of routine testing and the assumption that the virus is primarily a concern for poultry, recent studies suggest that H5N1 can infect a wide range of animals, including mammals, and may pose a greater risk to humans than previously thought.
Farmworkers at Risk
Farmworkers, particularly those in close contact with infected animals, are at risk of exposure to H5N1. However, there is currently no systematic testing in place to monitor these workers for potential infections. This lack of surveillance means that cases of human infection may go undetected, posing a silent threat to public health.
Investigating H5N1 on Texas Dairy Farms
In early April 2024, researchers from the University of Texas Medical Branch conducted a study on two dairy farms in Texas that had recently experienced outbreaks of H5N1 HPAIV. The farms, referred to as Farm A and Farm B, were selected for their significant animal losses and the presence of respiratory illness among their cattle.
Methodology
The researchers employed a range of advanced techniques, including molecular assays, cell and egg culture, and both Sanger and next-generation sequencing, to analyze samples collected from the farms. These samples included cow nasal swabs, milk specimens, fecal slurry, and an oropharyngeal and cloacal swab from a dead bird found on one of the farms.
Key Findings
The study's results were striking. H5N1 HPAIV was detected in 64% of milk samples and 2.6% of cattle nasal swabs.
Surprisingly, none of the nasopharyngeal swabs from farmworkers tested positive for the virus.
Despite this, serological tests revealed that 14.3% of the farmworkers had elevated neutralizing antibodies against a related H5N1 strain, indicating that they had been exposed to the virus.
The virus was successfully cultured and characterized from several samples, and sequencing showed that the strains were closely related to other recent H5N1 strains circulating in Texas. Additionally, one of the nasal swabs from a sick cow tested positive for SARS-CoV-2, highlighting the potential for co-infection and the complexity of managing viral outbreaks on farms.
Environmental Contamination
The investigation also
found evidence of H5N1 in the farm environment, including a fecal slurry sample. This underscores the potential for environmental transmission of the virus and the need for comprehensive biosecurity measures to prevent the spread of H5N1 on farms.
Implications for Public Health
The findings from this study are significant for several reasons. First, they demonstrate that H5N1 HPAIV can infect cattle and persist in their milk, posing a risk for zoonotic transmission to humans. This has been covered extensively in various past
H5N1 News coverages but there were attempts to downplay this by the USDA who claims that the current pasteurization methods can inhibit the virus. There are however newer studies that such current methods employed by many companies might not suffice and furthermore even degraded viral peptides found in the milk could possibly be harmful to human health.
https://www.thailandmedical.news/news/new-study-challenges-usda-and-u-s-fda-claims-on-safety-of-pasteurized-milk-from-h5n1-infected-cows
https://www.thailandmedical.news/news/most-unaware-that-junk-viral-peptides-produced-during-replication-are-pathogenic-and-can-withstand-temperatures-above-70-degrees-celsius
https://www.thailandmedical.news/news/infected-cows-can-produce-milk-that-has-a-changed-composition-which-can-affect-human-health
Second, the detection of antibodies in farmworkers suggests that human exposure to the virus may be more common than previously thought, even in the absence of symptomatic illness. This has important implications for occupational health and safety practices on farms, highlighting the need for regular monitoring and protective measures for workers.
The presence of H5N1 in milk also raises concerns about the potential for the virus to enter the food supply. While there is currently no evidence that H5N1 can be transmitted through consumption of dairy products, the possibility cannot be entirely ruled out, underscoring the importance of rigorous testing and safety protocols.
The One Health Approach
This investigation exemplifies the One Health approach, which recognizes the interconnectedness of human, animal, and environmental health. By studying the transmission of H5N1 HPAIV in a real-world farm setting, the researchers have highlighted the importance of integrated surveillance and response strategies to control the spread of zoonotic diseases. This approach is critical in preventing future outbreaks and protecting both human and animal health.
Broader Context: Mammal Infections
The study in Texas is part of a larger trend of H5N1 infections in a variety of mammal species. According to the Centers for Disease Control and Prevention (CDC), the spread of H5N1 among wild birds has led to infections in mammals, including foxes, bears, and even seals. These events suggest that the virus can adapt to infect mammals more efficiently, potentially increasing the risk of human infection.
Mammal Infections and Public Health
The detection of H5N1 in a range of mammal species is concerning for several reasons. First, it indicates that the virus is capable of crossing species barriers, which could facilitate its spread to humans. Second, infections in mammals often result in severe disease, which could increase the virus's pathogenicity if it were to infect humans. Finally, the spread of H5N1 in mammals suggests that the virus is undergoing genetic changes that may enhance its ability to infect new hosts.
Future Directions
The study authors emphasize the need for further research to understand the dynamics of H5N1 HPAIV transmission on farms. They call for more comprehensive epidemiological studies to quantify the extent of viral shedding in cattle and the duration of virus presence in milk. Additionally, they advocate for improved biosecurity measures and regular health monitoring of farmworkers to prevent zoonotic transmission.
Enhanced surveillance is also needed to monitor the spread of H5N1 among wild birds and mammals. This will help identify potential outbreaks early and allow for prompt intervention to prevent the virus from spreading to new areas or hosts.
Vaccine Development
Given the potential for H5N1 to infect humans, the development of effective vaccines is a priority. Current efforts are focused on creating vaccines that can provide broad protection against multiple strains of H5N1. These vaccines would be valuable not only for protecting at-risk populations, such as farmworkers, but also for preventing the spread of the virus in the event of an outbreak.
Conclusion
The detection of H5N1 HPAIV on Texas dairy farms and the evidence of human exposure underscore the urgent need for enhanced surveillance and biosecurity measures to protect public health. This study highlights the potential for undetected transmission of avian influenza viruses and the importance of the One Health approach in addressing zoonotic disease threats. As we continue to face emerging infectious diseases, integrated efforts to monitor and control these threats are more critical than ever.
The broader context of H5N1 infections in mammals further emphasizes the need for vigilant surveillance and prompt response to prevent the virus from spreading to new hosts and potentially causing a human pandemic. By taking a proactive approach and prioritizing research, surveillance, and vaccine development, we can better protect both human and animal health from the threat of H5N1 and other emerging infectious diseases.
The research findings were published on a preprint server and are currently being peer reviewed.
https://www.medrxiv.org/content/10.1101/2024.07.27.24310982v1
For the latest
H5N1 News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/breaking-h5n1-genotype-affecting-cows-in-america-possibly-gains-entry-into-humans-via-the-eyes-thru-the-new-pb2-e67k-mutation
https://www.thailandmedical.news/news/warning-h5n1-and-other-avian-flu-viruses-can-be-spread-by-insects-such-as-mosquitoes-house-flies-beetles-cockroaches-etc
https://www.thailandmedical.news/news/breaking-highly-pathogenic-avian-influenza-viruses-such-as-h5n1-are-also-wind-borne-and-can-be-transmitted-over-distances-of-up-to-25-km