Study Shows That Individuals With Only Mild SARS-CoV-2 Infections Can Still Shed Virus For longer Periods With One Case Study As Long As Eight Months!
Source: SARS-CoV-2 Viral Shedding Jan 28, 2022 3 years, 2 months, 3 weeks, 3 days, 5 hours, 48 minutes ago
SARS-CoV-2 Viral Shedding: Researchers from the University of São Paulo-Brazil and the Institut Pasteur, Paris-France have in a new study found that some individuals can still continue to shed the SARS-CoV-2 coronavirus over very long periods despite only manifesting mild symptoms upon initial infection. One case study even showed an individual continue to shed the virus for as long as eight months!
The SARS-CoV-2 infection is caused by a respiratory pathogen with a wide range of manifestations, varying from asymptomatic to fatal cases, with a generally short outcome. However, some individuals present long-term viral shedding.
The study team monitored 38 individuals who were mildly affected by the SARS-CoV-2 infection. Out of the total studied population, three (7.9%) showed atypical events regarding the duration of positivity for viral RNA detection.
In one of these atypical cases, a previously HIV-positive male patient presented a SARS-CoV-2 RNA shedding and subgenomic RNA (sgRNA) detected from the upper respiratory tract, respectively, for 232 and 224 days after the onset of the symptoms.
The SARS-CoV-2 B.1.1.28 lineage, one of the most prevalent in Brazil in 2020, was identified in this patient in three serial samples. Interestingly, the genomic analyses performed throughout the infectious process showed an increase in the genetic diversity of the B.1.1.28 lineage within the host itself, with viral clearance occurring naturally, without any intervention measures to control the infection.
Contrasting widely spread current knowledge, the study findings indicate that potentially infectious SARS-CoV-2 virus might be shed by much longer periods by some infected patients. This data call attention to better adapted non-pharmacological measures and clinical discharge of patients aiming at preventing the spread of SARS-CoV-2 to the population.
The study findings were published in the peer reviewed journal: Frontiers In Medicine.
https://www.frontiersin.org/articles/10.3389/fmed.2021.760170/full
In one case study involving a 38-year-old man who manifested mild symptoms of COVID-19 for 20 days, the novel coronavirus continued to be detected in his body while undergoing mutations for as long as 232 days. The physicians warned that if he had not been given continuous medical care, maintained social distancing and worn a mask, he could have spread the virus throughout these seven months.
This atypical case of infection by SARS-CoV-2 was part of a study involving 38 Brazilian patients followed on a weekly basis between April and November 2020 by the study team.
The patients were followed until they tested negative twice or three times consecutively by RT-qPCR.
The
SARS-CoV-2 Viral Shedding study findings serve as an alert regarding the risk of limiting quarantine for COVID-19 patients to seven, ten or even 14 days after they test positive, as initially prescribed by protocols to combat the disease. It also reinforces the significance of vaccination, social distancing, and mask wearing.
;
Interestingly, of the 38 cases we tracked, two men and a woman were atypical in the sense that the virus was continuously detected in their organism for more than 70 days.
First author, Dr Marielton dos Passos Cunha from University of São Paulo told Thailand Medical News, “From the study findings, it can be said that about 8% of people infected by SARS-CoV-2 may be able to transmit the virus for more than two months, without necessarily manifesting any symptoms during the final stage of the infection."
The research was conducted while Dr Passos Cunha was a postdoctoral intern at the Pasteur-USP Scientific Platform.
Dr Paola Minoprio, one of the principal investigators for the study added, "We wanted to know if a period of 14 days was really long enough for the virus to stop being detectable. We concluded that it wasn't. It can take a month for a patient to test negative, and in some cases included in our study the patients remained positive for 71 to 232 days."
It should be noted that this is not the first evidence that the virus can remain active for longer than expected even in patients with mild symptoms. In early 2021, researchers at the University of São Paulo's Institute of Tropical Medicine (IMT-USP) in Brazil analyzed 29 samples of nasopharyngeal secretion from patients who tested positive for COVID-19. The material was collected at a public primary health center on the tenth day after the onset of symptoms, and inoculated into laboratory-grown cells. In 25% of the cases, the viruses present in the samples were capable of infecting the cells and replicating in vitro.
https://agencia.fapesp.br/study-suggests-shortening-quarantine-for-people-infected-by-novel-coronavirus-to-ten-days-would-be-risky/35303/
Hence in theory, therefore, other individuals could be infected if they came into contact with droplets of saliva expelled by 25% of these patients at the time the material was collected.
It has also been found that the risk appears to be even greater for people with compromised immune systems. In a paper published in June 2021, researchers at the same university's Medical School (FM-USP) described a case of infection that lasted at least 218 days. The patient was about 40 years old and had undergone aggressive treatment for cancer before contracting COVID-19.
https://agencia.fapesp.br/sars-cov-2-continued-to-replicate-and-mutate-in-a-patient-for-218-days/36281/
Yet another clinical case report published in the New England Journal of Medicine in early December 2020 reported the case of an immunocompromised 45-year-old man with an autoimmune blood disorder in whom the virus continued to replicate for 143 days.
https://www.nejm.org/doi/full/10.1056/nejmc2031364
Another case study published in Cell journal in late December 2020 outlined a case study of a female leukemia patient in whom the virus continued to replicate for at least 70 days, although she had no symptoms of COVID-19.
https://www.cell.com/cell/fulltext/S0092-8674(20)31456-2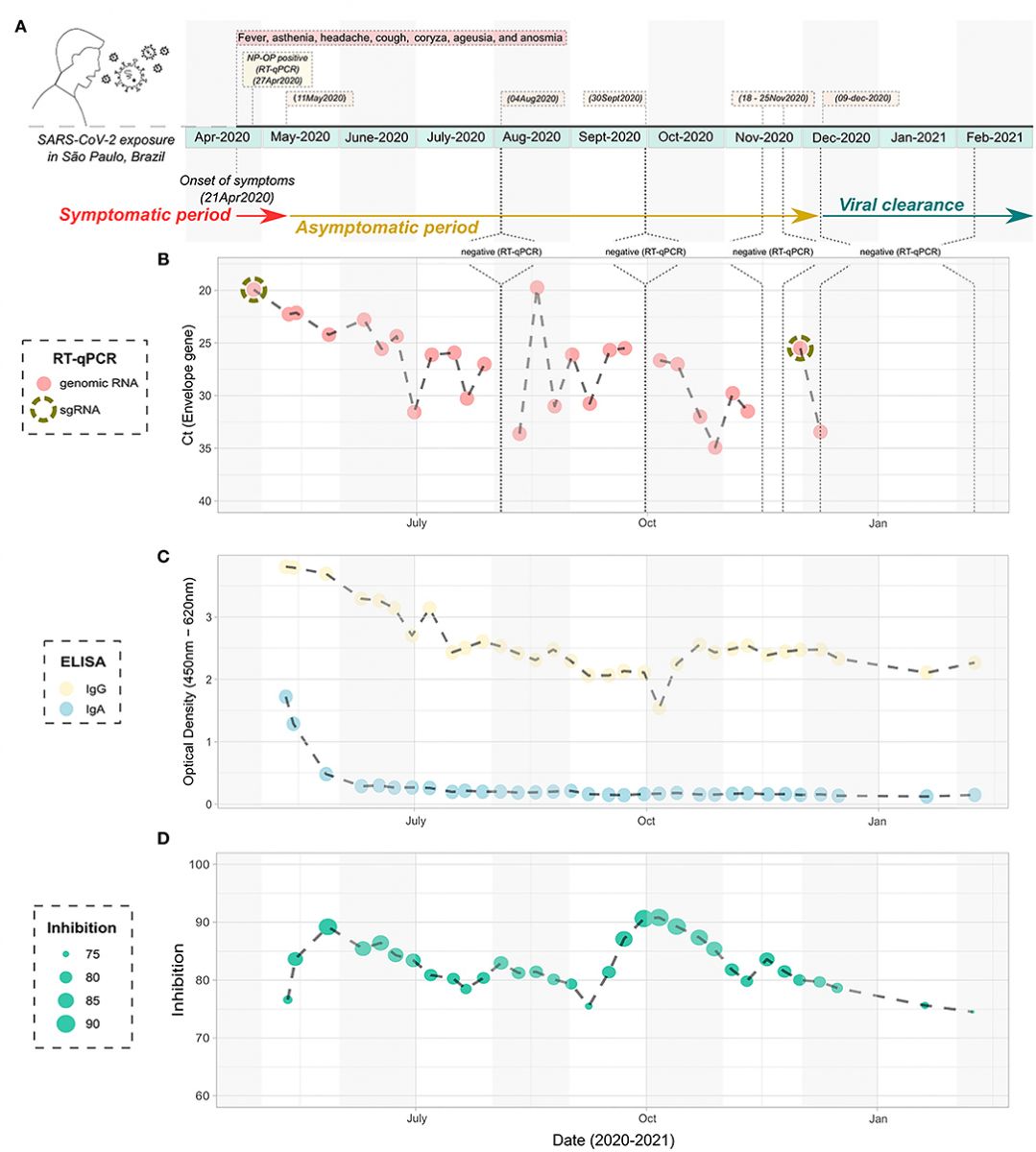 Timeline infection of the atypical studied patient with prolonged detection of viral RNA. (A) Schematic figure containing the diagnostic points, harvesting, and symptoms over time. (B) Cycle threshold to the Envelope gene of the SARS-CoV-2 according to the timeline of infection, as determined by RT-qPCR. The NP-OP swabs positive to the detection of subgenomic RNA are indicated by the dashed circle. (C) ELISA data showing the detection of IgA and IgG specific anti- SARS-CoV-2 nucleocapsid according to the timeline of infection. (D) Inhibition of the SARS-CoV-2/ACE2 ligation mediated by receptor-binding domain by neutralizing antibodies, according to the timeline of infection. SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; NP-OP, nasopharyngeal-oropharyngeal; ELISA, enzyme-linked immunosorbent assay.
Timeline infection of the atypical studied patient with prolonged detection of viral RNA. (A) Schematic figure containing the diagnostic points, harvesting, and symptoms over time. (B) Cycle threshold to the Envelope gene of the SARS-CoV-2 according to the timeline of infection, as determined by RT-qPCR. The NP-OP swabs positive to the detection of subgenomic RNA are indicated by the dashed circle. (C) ELISA data showing the detection of IgA and IgG specific anti- SARS-CoV-2 nucleocapsid according to the timeline of infection. (D) Inhibition of the SARS-CoV-2/ACE2 ligation mediated by receptor-binding domain by neutralizing antibodies, according to the timeline of infection. SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; NP-OP, nasopharyngeal-oropharyngeal; ELISA, enzyme-linked immunosorbent assay.
Despite all this existing evidence, the Brazilian Ministry of Health this week reduced the recommended period of self-isolation from ten to seven days for patients with mild or moderate symptoms, and to five days for people without symptoms if they test negative.
It should be noted that America was the one that started this trend as at end-2021, the US Centers for Disease Control and Prevention (CDC) cut its recommendation from ten to five days in the case of asymptomatic patients provided they continue to wear a mask and test negative for COVID-19.
In this same study, the difference between women and men in terms of the duration of viral activity was not significant (averaging 22 days and 33 days respectively). As for the three atypical cases, the virus remained detectable for 71 days in the woman and 81 days in one of the two men. None of them had comorbidities and all had mild symptoms of COVID-19.
Intra-Host SARS-CoV-2 Evolution
The atypical case patient, a male continued to test positive for coronavirus for 232 days (April-November 2020), after which he tested negative three times by RT-qPCR. He has had HIV, the virus that causes AIDS, since 2018 but has no detectable viral load thanks to antiretroviral therapy.
Dr Minoprio added, "The fact that he's seropositive for HIV doesn't mean he's more susceptible to other infections, as he has undergone the therapy since he was diagnosed. His capacity to respond to an infection by another agent is comparable to that of any other individual, and indeed he did respond to coronavirus when infected. He isn't immunosuppressed like cancer patients, people with autoimmune diseases or transplantees, for example."
The study tea said that his HIV-positive status does not explain the long duration of his coronavirus infection. Many patients infected concurrently by HIV and SARS-CoV-2 would have to be compared with an appropriate control group in order to see if any genetic or immune traits in the host could be associated with such prolonged viral shedding.
This male patient underwent weekly tests that detected the persistence of the infection, and samples of the virus were regularly sequenced to show that it was not a case of reinfection and that the virus not only continued to replicate but was also mutating.
Importantly, the strategies used by the virus to escape the immune system during the infection were mapped, showing that viral load fell when there were more neutralizing antibodies, and that the virus was able to circumvent the body's defenses to build the load up again. The cycle repeated, forcing the production of more antibodies until viral load was again reduced.
Dr Passos Cunha added, "It's important to observe patients like this one because we can learn more about how the virus mutates and which mutations can give rise to variants of concern.”
This male patient in the study was infected by lineage B.1.1.28, which entered Brazil at the start of 2020. The study team did not detect mutations in the virus isolated from the patient that could justify classifying it as more transmissible or more resistant to the immune system.
It should be noted that the University of São Paulo-Brazil and the Institut Pasteur research platform continues to investigate these and other cases.
All the 38 patients analyzed in the study led by Dr Minoprio are part of a bank of blood and nasopharyngeal secretion samples collected from 721 people who manifested symptoms associated with this coronavirus.
Dr Passos Cunha added, "Fresh data will come from these samples, and we might be able to produce more palpable explanations for these atypical cases.”
Dr Minoprio stressed, “Importantly these cases are further evidence that mask wearing and social distancing are the best ways to control the pandemic. If 14 days after testing positive a person isn't tested again, they may still be shedding active viruses and be able to infect others, contributing to community transmission, It is also crucial to keep track of infected people so we can find out more about mutations, novel variants, and the transmissibility of SARS-CoV-2."
The study team also stressed, “Since the severity of the clinical condition of patients with COVID-19 or the resistance status to the infection is previously shown to be associated with a genetic background of the host, it could also be hypothesized that the prolonged viral shedding is related to the host genetic environment. Still, genetic factors associated with the SARS-CoV-2 viruses or specific for certain viral lineages could certainly influence viral shedding. Other linked factors to the host, such as age, other comorbidities association, nutritional state, and previous exposure to different pathogens, could interfere with such a differential behavior of the SARS-CoV-2 during the infectious process and affect healing and transmission.”
For more about
SARS-CoV-2 Viral Shedding, keep on logging to Thailand Medical News.
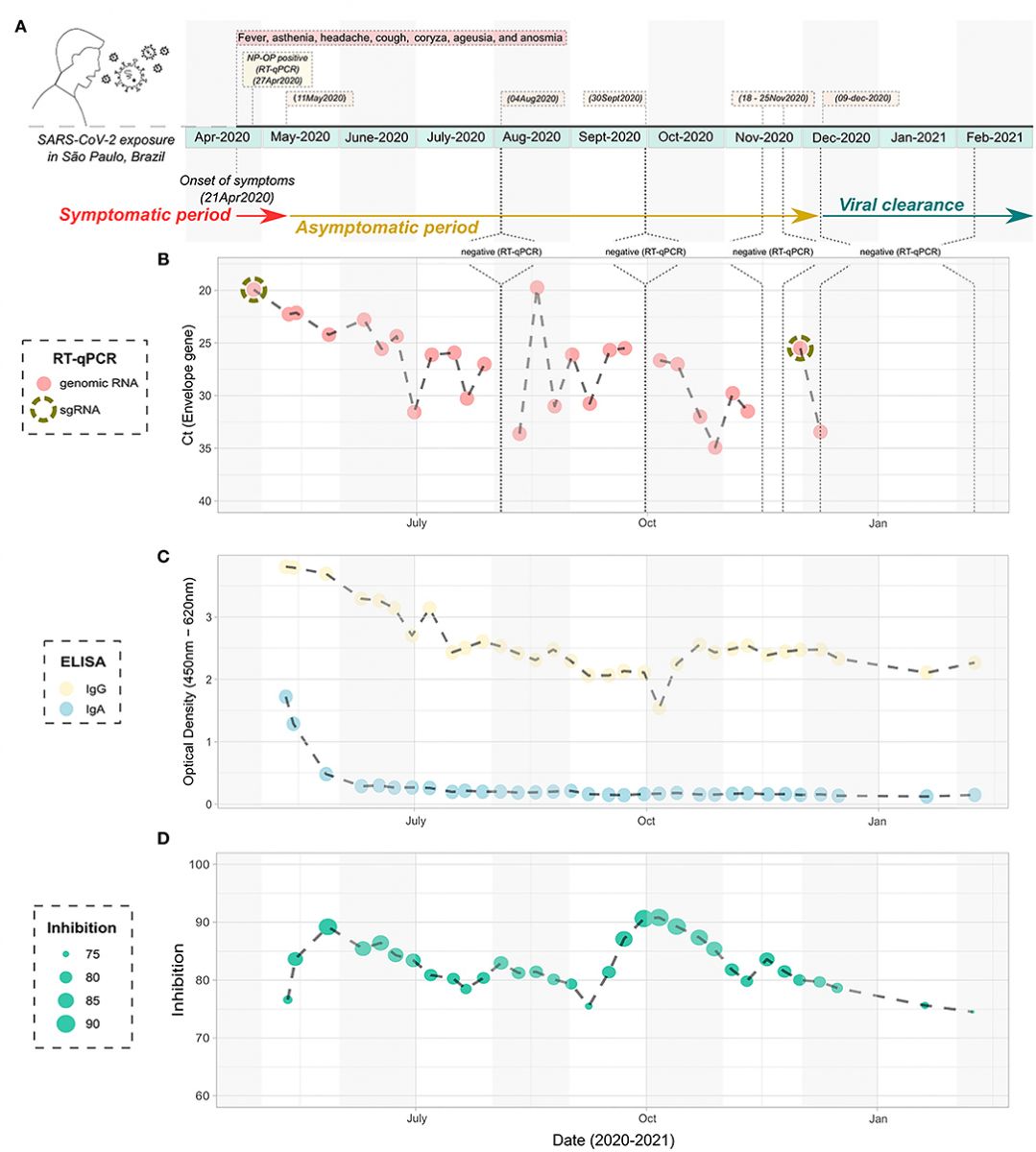 Timeline infection of the atypical studied patient with prolonged detection of viral RNA. (A) Schematic figure containing the diagnostic points, harvesting, and symptoms over time. (B) Cycle threshold to the Envelope gene of the SARS-CoV-2 according to the timeline of infection, as determined by RT-qPCR. The NP-OP swabs positive to the detection of subgenomic RNA are indicated by the dashed circle. (C) ELISA data showing the detection of IgA and IgG specific anti- SARS-CoV-2 nucleocapsid according to the timeline of infection. (D) Inhibition of the SARS-CoV-2/ACE2 ligation mediated by receptor-binding domain by neutralizing antibodies, according to the timeline of infection. SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; NP-OP, nasopharyngeal-oropharyngeal; ELISA, enzyme-linked immunosorbent assay.
Timeline infection of the atypical studied patient with prolonged detection of viral RNA. (A) Schematic figure containing the diagnostic points, harvesting, and symptoms over time. (B) Cycle threshold to the Envelope gene of the SARS-CoV-2 according to the timeline of infection, as determined by RT-qPCR. The NP-OP swabs positive to the detection of subgenomic RNA are indicated by the dashed circle. (C) ELISA data showing the detection of IgA and IgG specific anti- SARS-CoV-2 nucleocapsid according to the timeline of infection. (D) Inhibition of the SARS-CoV-2/ACE2 ligation mediated by receptor-binding domain by neutralizing antibodies, according to the timeline of infection. SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; NP-OP, nasopharyngeal-oropharyngeal; ELISA, enzyme-linked immunosorbent assay.