Thailand Medical Experts Announce New Nuclear Medicine Guidelines for Dementia Diagnosis
Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 07, 2024 5 months, 1 week, 6 days, 11 hours, 4 minutes ago
Thailand Medical: A collaboration among Thailand's leading medical experts and communities has produced new guidelines on using nuclear medicine to diagnose neurocognitive disorders like dementia. Spearheaded by the Nuclear Medicine Society of Thailand, the Neurological Society of Thailand, and the Thai Medical Physicist Society, these guidelines outline the critical role of PET and SPECT imaging in diagnosing dementia, allowing doctors to detect signs earlier and make informed treatment plans.
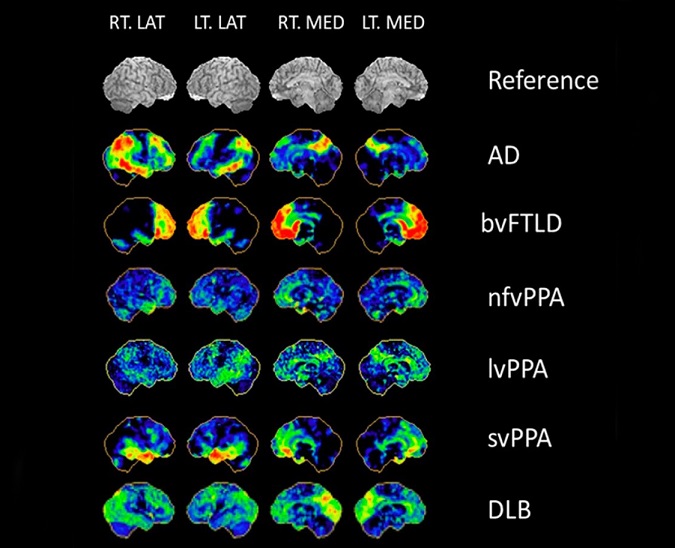
 3D-SSP of dementia syndrome. Courtesy: Professor Satoshi Minoshima, modified with permission. LT = left, RT = right, LAT = lateral view, MED = medial view, AD = Alzheimer’s disease, bvFTLD = behavioral variant FTD, nfvPPA = non-fluent variant primary progressive aphasia, lvPPA = logopenic variant primary progressive aphasia, svPPA = semantic variant primary progressive aphasia, DLB = dementia with Lewy bodies. Color shows the specific hypometabolic brain region in each type of dementia
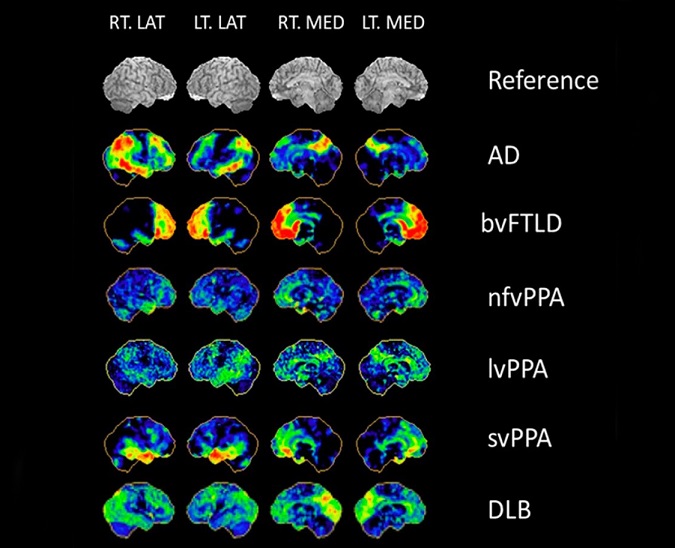
3D-SSP of dementia syndrome. Courtesy: Professor Satoshi Minoshima, modified with permission. LT = left, RT = right, LAT = lateral view, MED = medial view, AD = Alzheimer’s disease, bvFTLD = behavioral variant FTD, nfvPPA = non-fluent variant primary progressive aphasia, lvPPA = logopenic variant primary progressive aphasia, svPPA = semantic variant primary progressive aphasia, DLB = dementia with Lewy bodies. Color shows the specific hypometabolic brain region in each type of dementia
Nuclear medicine has long played a role in diagnosing complex brain disorders, such as Alzheimer’s disease. However, this
Thailand Medical News report explains, Thailand’s current guidelines emphasize not only the best practices for using these technologies but also aim to make access to proper diagnostic procedures easier for patients in need.
Importance of Early Diagnosis in Dementia
With dementia cases on the rise, Thailand faces a pressing demand for effective diagnostic tools. Dementia is not just memory loss but affects cognitive abilities, such as judgment, language, and problem-solving. Early detection is essential, as it allows more personalized treatments and interventions that may slow the disease’s progression. The new guidelines detail a sequence for selecting the most appropriate tests, depending on the symptoms and needs of each patient.
Researchers from Chiang Mai University, Siriraj Hospital, Chulalongkorn University, Khon Kaen University, and King Chulalongkorn Memorial Hospital collaborated on these guidelines, highlighting specific nuclear medicine tests’ usefulness for particular types of dementia, such as Alzheimer’s and Lewy Body dementia. These studies clarify how each imaging type, PET or SPECT, brings unique insights, helping doctors spot abnormalities that traditional scans like MRI or CT might miss.
Detailed Recommendations for Using PET and SPECT
The guidelines advise doctors on which nuclear imaging technique to use depending on the type of dementia suspected. PET (Positron Emission Tomography) and SPECT (Single-Photon Emission Computed Tomography) are both recommended for different scenarios. PET scans detect metabolic brain changes, while SPECT focuses on blood flow. These techniques complement each other by revealing both structural and molecular changes in the brain.
-PET and SPECT: PET, particularly using FDG (fluorodeoxyglucose), helps reveal patterns of brain glucose metabolism and is beneficial in diagnosing Alzheimer's early.
For conditions like Lewy Body dementia, PET can be paired with other tests to differentiate between types. SPECT, on the other hand, offers insight into blood flow within the brain and is frequently used for diagnosing vascular dementia.
-Specificity for Different Dementias: The guidelines specify which scan works best for each type of dementia. For instance, brain hypometabolism patterns observed in Alzheimer's patients are different from the brain activity seen in those with vascular dementia. This specificity helps doctors better distinguish between these disorders.
Practical Steps for Clinicians
The guidelines cover a step-by-step approach for clinicians, from patient preparation to imaging and reporting. Doctors are advised to review a patient's history and current medications, as certain substances, such as caffeine or nicotine, can affect scan results. In cases where metabolic rates need measuring, PET scans with FDG are recommended. Conversely, SPECT scans may be preferable for assessing cerebral blood flow.
Researchers have also recommended standard radiopharmaceutical doses for these procedures, ensuring consistency and reliability in test results across different facilities. These guidelines emphasize the importance of patient comfort and safety, particularly since some patients may require sedation.
Expanded Findings and Implications
One remarkable finding from these guidelines is the proposed sequence of tests that increase diagnostic accuracy while keeping costs manageable. Nuclear imaging techniques are expensive and not widely available across Thailand. Therefore, the guidelines suggest a structured flowchart for selecting procedures, ensuring each test is used only when it offers significant diagnostic value.
Additionally, these guidelines address common issues in interpreting PET and SPECT results, providing doctors with tools to differentiate between similar dementia types. For example, a unique “Z-score” mapping system can visually illustrate affected brain regions, helping even less experienced nuclear medicine professionals identify dementia patterns accurately.
New Directions in Nuclear Medicine and Dementia Care
The guidelines also touch on emerging technologies, such as amyloid PET and tau imaging. Amyloid PET helps visualize plaques associated with Alzheimer's, while tau PET highlights the spread of neurofibrillary tangles. These advancements have exciting potential for research and treatment.
The recommendations advise caution, noting that while amyloid PET scans can confirm the presence of plaques, they do not alone diagnose Alzheimer’s. This added layer of imaging may become a valuable resource as more facilities across Thailand acquire this technology. Notably, they recommend combined imaging approaches for complex cases, such as using PET and MRI together for a more comprehensive view.
Conclusion: Streamlining Nuclear Imaging for Thailand’s Aging Population
In conclusion, the new guidelines from Thailand’s top medical societies simplify the nuclear imaging process, making it accessible and efficient for diagnosing dementia. By following a structured approach to nuclear medicine, doctors can make earlier and more accurate diagnoses, potentially improving life quality for Thailand’s elderly population facing cognitive decline.
These guidelines serve as a significant step forward, particularly as Thailand’s population continues to age and dementia cases rise. By offering clear, evidence-based recommendations, doctors across the country are better equipped to support patients with neurocognitive disorders. With nuclear imaging now firmly part of the diagnostic toolkit, Thai physicians can make informed choices that benefit patients and families alike.
The study findings and guidelines were published in the peer-reviewed journal: Diagnostics.
https://www.mdpi.com/2075-4418/14/22/2474
For the latest on Nuclear Medicine, keep on logging to
Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/new-thailand-medical-study-reveals-link-between-oral-microbiota-and-alzheimer-s-disease
https://www.thailandmedical.news/news/canadian-study-finds-that-insulin-resistance-in-the-brain-contributes-to-cognitive-decline-and-psychiatric-issues
https://www.thailandmedical.news/news/thailand-medical-researchers-find-that-huperzine-a-from-huperzia-serrata-moss-can-help-combat-alzheimer-s-disease