Thailand medical study finds that treating COVID-19 patients with corticosteroids increases risk of Tuberculosis
Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 21, 2024 5 months, 4 weeks, 2 days, 12 hours, 4 minutes ago
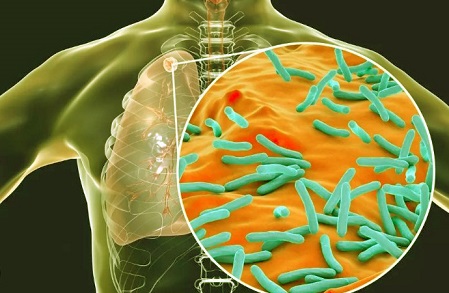
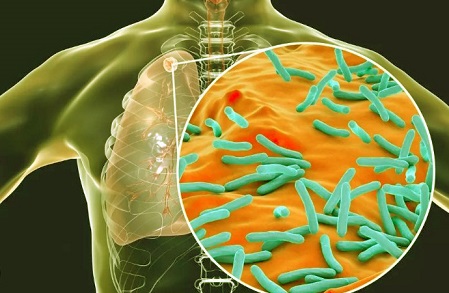
Thailand Medical: A recent study conducted by researchers from King Chulalongkorn Memorial Hospital and the Thai Red Cross Society in Thailand has found a significant connection between high doses of corticosteroids used to treat severe COVID-19 pneumonia and the increased risk of developing active pulmonary tuberculosis (TB). The researchers from the Faculty of Medicine at Chulalongkorn University investigated the impact of these powerful anti-inflammatory drugs on the incidence of TB among COVID-19 patients, uncovering alarming statistics that suggest caution in the use of corticosteroids for individuals with certain risk factors.
 Thailand medical study finds that treating COVID-19 patients with corticosteroids
Thailand medical study finds that treating COVID-19 patients with corticosteroids
increases risk of Tuberculosis
Steroids and COVID-19: A Double-Edged Sword
Corticosteroids, such as dexamethasone, have been widely used to reduce inflammation and improve outcomes in patients suffering from severe COVID-19 pneumonia. These drugs, often lifesaving in the short term, suppress the immune system, allowing the body to heal by reducing overactive immune responses like the cytokine storm seen in severe cases of COVID-19. However, this
Thailand Medical study addresses the growing concern over opportunistic infections, especially tuberculosis, among patients receiving high doses of these immunosuppressive drugs.
The researchers undertook this study to fill a knowledge gap regarding whether high-dose corticosteroid therapy for COVID-19 pneumonia increases the likelihood of subsequent TB infection, especially given that tuberculosis is an endemic disease in many regions, including Thailand.
Study Findings
The study, which spanned from October 2022 to June 2023, involved 243 participants who had been diagnosed with COVID-19 and were treated with high doses of corticosteroids. It was found that patients on corticosteroids had a significantly higher chance of developing TB within the year following their COVID-19 diagnosis.
Among the participants, 1.6% (4 out of 243) were diagnosed with active TB within a year, translating to an incidence rate of 1,646 cases per 100,000 person-years - an incidence rate 11 times higher than that of the general population. The study highlighted that individuals with chronic conditions like chronic kidney disease (CKD) and chronic lung diseases were particularly vulnerable to contracting TB after receiving high-dose corticosteroids for COVID-19.
These findings stress the importance of vigilant monitoring and possibly screening for latent TB in COVID-19 patients, particularly those who require corticosteroid therapy.
Risk Factors Identified
The study also delved into the characteristics of patients who were more likely to develop TB after COVID-19. It found that the elderly, particularly those aged 75 and above, were at higher risk. Additionally, individuals with a history of chronic lung diseases like chronic obstructive pulmonary disease (COPD) and those with CKD were more susceptible to de
veloping active TB.
Interestingly, although diabetes mellitus has traditionally been considered a risk factor for TB, this study did not find a statistically significant link between diabetes and subsequent TB infection in COVID-19 patients on corticosteroids.
The mortality rate among those who developed TB after receiving corticosteroid treatment for COVID-19 was also significantly higher - 50% - compared to just 0.4% in patients who did not develop TB. This underscores the lethal consequences of co-infection in vulnerable individuals.
Opportunistic Co-Infections
Beyond TB, the study found that patients on high doses of corticosteroids were at risk of other opportunistic infections. Co-infections with bacteria, fungi, and Pneumocystis jirovecii (PJP) were observed in many participants, with bacterial infections being the most common. Around 37.1% of patients were co-infected with bacteria, 5.3% with fungi, and 1.2% with PJP. The most frequently identified bacterial pathogens were Klebsiella pneumoniae, Escherichia coli, and Pseudomonas aeruginosa. Fungal infections primarily involved Aspergillus spp., which were more prevalent than Candida spp..
The presence of these co-infections further complicated the clinical management of COVID-19 patients, particularly those on corticosteroid therapy. The researchers recommend heightened awareness and early diagnosis of these infections to prevent adverse outcomes.
Recommendations and Future Considerations
Given the findings, the researchers recommend that clinicians treating COVID-19 patients with high-dose corticosteroids should consider screening for latent TB, especially in individuals with pre-existing conditions like CKD and chronic lung diseases. Early screening and diagnosis could help prevent the progression of latent TB into an active disease, reducing mortality and improving outcomes in this vulnerable patient group.
Additionally, while corticosteroids remain a valuable tool in managing severe COVID-19 cases, the study highlights the importance of balancing the benefits of reducing inflammation against the risk of suppressing the immune system too much. Clinicians are urged to use these drugs judiciously, particularly in populations that are at higher risk for TB and other opportunistic infections.
Conclusions
This study makes it clear that while corticosteroids are effective in reducing the inflammation associated with severe COVID-19 pneumonia, their use comes with substantial risks, particularly in regions where tuberculosis is endemic. The incidence of TB among COVID-19 patients on high-dose corticosteroids is significantly higher than in the general population, and the associated mortality rates are concerning.
The findings suggest that routine screening for latent TB in high-risk COVID-19 patients, particularly those with chronic conditions or the elderly, could be beneficial in preventing the development of active TB and reducing the associated mortality. Additionally, the increased incidence of opportunistic infections like aspergillosis and PJP calls for greater vigilance and possibly preventive measures in patients receiving immunosuppressive therapy for COVID-19.
The study findings were published in the peer-reviewed journal PLOS ONE.
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0309392
For the latest research news, keep on logging to
Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/sunday-editorial-covid-19-could-possibly-be-contributing-directly-and-indirectly-to-the-rise-of-tuberculosis-infections
https://www.thailandmedical.news/news/medical-thailand-thai-study-validates-that-covid-19-induced-immune-dysfunction-is-driving-increased-incidence-of-pulmonary-tuberculosis