The COVID-19 Virus Exploits Host CD55, CD59, and Factor H to Evade Antibody-Dependent Complement-Mediated Lysis
Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 29, 2024 5 months, 2 weeks, 1 day, 7 minutes ago
Medical News: The human immune system has many defenses to protect against viruses and bacteria, and one of these is the complement system. It is a complex network of over 30 proteins in our blood and tissues that attack harmful pathogens. The system can destroy invaders by marking them for other immune cells to attack, calling for help from nearby cells, or directly breaking down the pathogens.
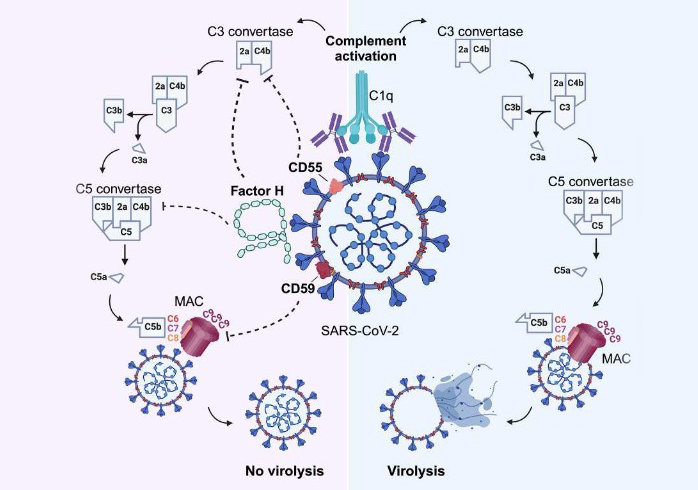
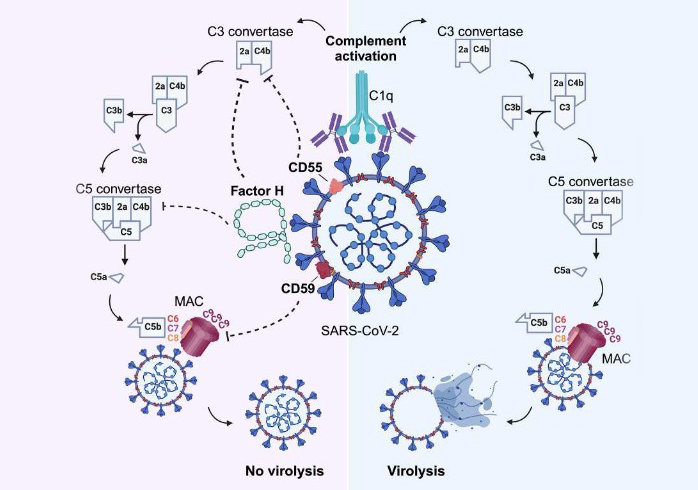 Graphical Abstract: The COVID-19 Virus Exploits Host CD55, CD59, and Factor H to Evade Antibody-Dependent Complement-Mediated Lysis
Graphical Abstract: The COVID-19 Virus Exploits Host CD55, CD59, and Factor H to Evade Antibody-Dependent Complement-Mediated Lysis
While the complement system is crucial for fighting off viruses and bacteria, it must be tightly regulated. Unchecked complement activity can lead to severe damage to our cells, potentially triggering excessive inflammation. To prevent this, our bodies have special proteins that control the complement system, including CD55, CD59, and Factor H. These proteins protect human cells from the complement system, and new research shows that the COVID-19 virus, known as SARS-CoV-2, has learned to use these protective proteins to its advantage.
COVID-19 Hijacks Host Defenses
A recent study led by researchers from the Medical University of Vienna, the Medical University of Innsbruck, and the CeMM Research Center for Molecular Medicine in Austria, has discovered that SARS-CoV-2 takes control of CD55, CD59, and Factor H to evade the immune system. This
Medical News coverage reports that by using these proteins, SARS-CoV-2 can shield itself from being attacked by the complement system, making it harder for our immune system to kill the virus.
CD55 and CD59 are proteins typically found on the surface of human cells. They work as “decoys,” telling the complement system to ignore the cells that display them, which prevents friendly fire. Factor H, on the other hand, is a circulating protein that further aids in suppressing the complement system. By hijacking these proteins, SARS-CoV-2 can make itself look like part of the body’s own cells, avoiding detection and destruction by the immune system.
Key Findings of the Study
Researchers found that SARS-CoV-2 particles gain access to CD55 and CD59 while leaving infected cells. Using laboratory methods like liquid chromatography and mass spectrometry, the scientists isolated and analyzed the viral particles. They discovered that SARS-CoV-2 incorporates CD55 and CD59 into its structure, decorating its surface with these immune-protecting proteins.
This study went a step further to confirm that these proteins shield SARS-CoV-2 from being destroyed by antibody-dependent complement-mediated lysis (ADCML). ADCML is a process where the immune system, guided by antibodies, marks the virus for elimination. However, because SARS-CoV-2 is “wearing” the CD55 and CD59 proteins, the complement system is tricked and fails to attack.
The researchers tested this defense mechanism by blocking the CD55 and CD59 proteins on the virus. When blocked, SARS-CoV-2 was more vulnerable to the complement system, suggesting these proteins play a critical role in the virus's survival.
&
lt;strong>Factor H's Role in SARS-CoV-2 Evasion
Apart from CD55 and CD59, the study also focused on Factor H, a protein that COVID-19 can bind to from human blood. This protein, typically meant to protect our own cells from being accidentally destroyed by the immune system, gets absorbed by the virus. Factor H then binds to SARS-CoV-2, adding another layer of defense that prevents the complement system from attacking the virus.
By examining the interactions with lab-made components of Factor H, called SCR18-20, the researchers demonstrated that this fragment of Factor H binds to the viral particles. The study found that when SARS-CoV-2 was exposed to Factor H inhibitors, the virus became vulnerable to the complement system. The findings underscore how Factor H strengthens SARS-CoV-2's defenses, adding to the virus’s ability to evade the immune system.
The Impact of the Complement System in COVID-19
The complement system is hyperactive in severe COVID-19 cases, which means it is working overtime, often leading to harmful inflammation in the body. The researchers explained that when SARS-CoV-2 enters the body, it creates a complicated response in which the immune system is both attacking and simultaneously failing to clear the virus.
The study suggests that SARS-CoV-2 not only triggers the complement system but manipulates it to avoid being cleared by the immune response. Instead of directly battling the virus, the complement system gets redirected towards causing excessive inflammation in the patient's tissues.
The Importance of Virus-Specific Antibodies
Interestingly, the study also found that the complement system’s ability to destroy the virus depends on specific antibodies. When researchers used blood from people who had COVID-19 antibodies, the complement system was more effective at breaking down the virus. But in samples without these antibodies, the virus remained largely intact, even when the complement system was active.
This finding suggests that an effective immune response to COVID-19 may depend not only on a working complement system but also on the presence of COVID-19-specific antibodies. These antibodies are generated either from vaccination or previous infection, helping the immune system recognize and destroy the virus faster.
Potential Implications and Future Research
This study brings new insight into how SARS-CoV-2 can cleverly use human proteins to defend itself. Understanding these mechanisms may open up new ways to fight COVID-19. Drugs could potentially target these hijacked proteins on the virus, making it more susceptible to the immune response. Another strategy could involve boosting the body's natural complement system response, using antibodies that enhance its ability to destroy the virus.
Further research is required to determine how these findings could translate into therapies. By interfering with the virus’s ability to use CD55, CD59, and Factor H, scientists might find new ways to counteract COVID-19’s defenses. Such interventions could be beneficial for severe COVID-19 cases, where inflammation and immune evasion are major complications.
Study Conclusion
In conclusion, SARS-CoV-2’s interaction with the human immune system is more complex than initially understood. By co-opting host proteins CD55, CD59, and Factor H, the virus can evade immune responses, allowing it to spread and cause damage in the body while delaying its destruction by the immune system. This complex strategy helps explain why COVID-19 can be so severe for some individuals. The study highlights the need for therapeutic approaches targeting this evasion mechanism, which may improve the outcomes for severe COVID-19 cases.
This research, conducted by teams from the Medical University of Vienna, Medical University of Innsbruck, and CeMM, gives a detailed look into SARS-CoV-2’s survival tactics, bringing science a step closer to finding effective treatments for COVID-19.
The study findings were published in the peer-reviewed journal: Emerging Microbes & Infections.
https://www.tandfonline.com/doi/full/10.1080/22221751.2024.2417868
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/cd55-protein-s-role-in-covid-19-lung-damage-and-ards-a-potential-therapeutic-target
https://www.thailandmedical.news/news/-sars-cov-2-upregulates-cd55-complement-regulator-and-prolongs-its-activation-causing-an-immune-dysfunction-that-contributes-to-disease-severity-in-so