Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 03, 2024 4 months, 1 week, 3 days, 8 hours, 31 minutes ago
Medical News: Unveiling the Mystery of Severe COVID-19
The fight against COVID-19 has brought about countless studies aiming to understand how this virus wreaks havoc on the human body. A groundbreaking study by researchers from Johns Hopkins University, the University of Pittsburgh, and the Children's Hospital of Philadelphia reveals new insights. Their research pinpoints how the overactivation of the Renin-Angiotensin-Aldosterone System (RAAS) during a severe COVID-19 infection leads to multiple organ damage and even death. This
Medical News report dives into their findings and explains their implications for patients and healthcare.
 The Deadly Connection of COVID-19 and RAAS Overactivation
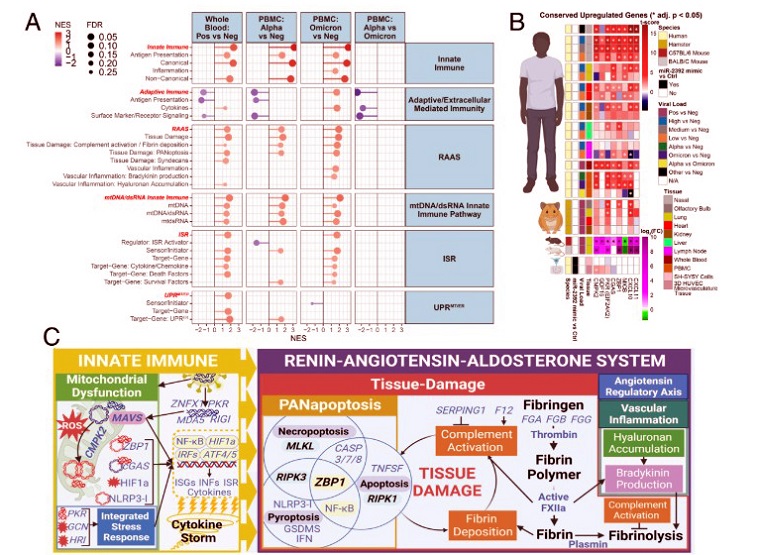
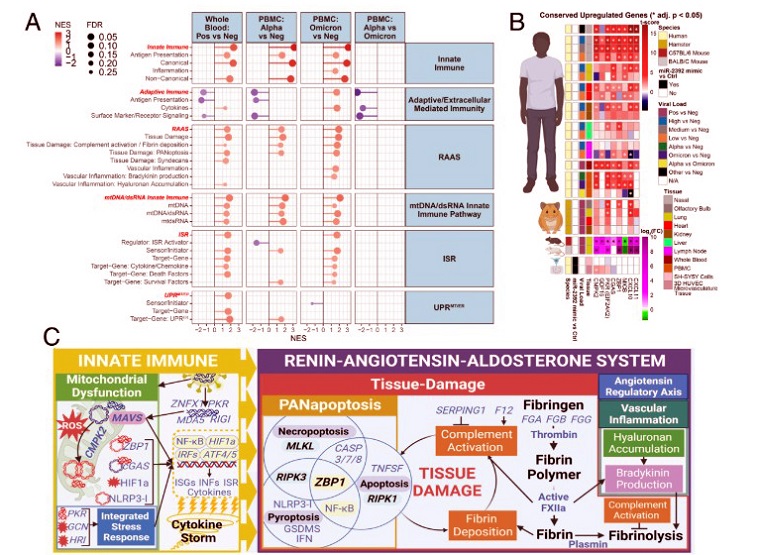
Transcript changes in PBMCs (Alpha and Omicron) and whole blood (Pre-Delta and Delta) display comparable immune responses. (A) Lollipop plots for statistically significant changes in custom gene sets determined by fGSEA for Whole blood and PBMCs ranked by NES. (B) Linear heatmap displaying the t-score statistics for conserved upregulated genes comparing PBMCs collected from SARS-CoV-2-Alpha and SARS-CoV-2-Omicron-infected patients versus non-infected patients. (C) Schematic summary figure of mtDNA/mtdsRNA-activated immune response with associated induction of EIF2AK2/PKR and ISR pathways driving dysfunctional RAAS pathway state.
The Deadly Connection of COVID-19 and RAAS Overactivation
Transcript changes in PBMCs (Alpha and Omicron) and whole blood (Pre-Delta and Delta) display comparable immune responses. (A) Lollipop plots for statistically significant changes in custom gene sets determined by fGSEA for Whole blood and PBMCs ranked by NES. (B) Linear heatmap displaying the t-score statistics for conserved upregulated genes comparing PBMCs collected from SARS-CoV-2-Alpha and SARS-CoV-2-Omicron-infected patients versus non-infected patients. (C) Schematic summary figure of mtDNA/mtdsRNA-activated immune response with associated induction of EIF2AK2/PKR and ISR pathways driving dysfunctional RAAS pathway state.
The scientists utilized RNA sequencing of nasal swabs and autopsied tissues from 40 patients who succumbed to COVID-19. They discovered that a group of immune and mitochondrial genes activates RAAS, triggering a cytokine storm - a surge of inflammatory responses - causing irreversible damage to the lungs, kidneys, heart, and liver. What stood out in this study was how RAAS overactivation undermines the function of mediastinal lymph nodes, central components of the immune system. This study explores these mechanisms, shedding light on the complexities of severe COVID-19.
Understanding RAAS and its Role in Inflammation
RAAS is a hormonal system that helps regulate blood pressure and fluid balance. It operates like a thermostat, adjusting as needed to maintain stability. However, in severe COVID-19 cases, this system spirals out of control. The virus reduces ACE2, a key receptor for SARS-CoV-2 and an essential regulator of RAAS. This reduction unleashes a cascade of harmful effects, including vascular leakage, clot formation, and tissue fibrosis.
In this study, the researchers identified 22 noncanonical immune genes - less commonly studied genes - that become overactive during COVID-19. These genes are associated with RAAS-related processes such as fibrin deposition, inflammation, and PANoptosis, a form of programmed cell death. They noted that severe cases often show a "bradykinin storm," where excessive bradykinin levels cause fluid buildup and inflammation in the lungs, leading to acute respiratory distress.
The Role of Mitochondrial Dysfunction
Mitochondria, the cell's energy powerhouses, are pivotal in immune regula
tion. In severe COVID-19, their dysfunction was linked to immune overreaction. Damaged mitochondria release mitochondrial DNA (mtDNA) and RNA into the cytoplasm, which the body mistakenly identifies as viral invaders. This misstep sets off inflammatory responses, compounding the damage to organs already weakened by the virus.
The study found elevated levels of mtDNA in lung, kidney, and heart tissues of COVID-19 victims, corroborating mitochondrial involvement in disease progression. In animal models, inhibiting this mitochondrial dysfunction reduced inflammation and improved survival rates, suggesting a potential therapeutic angle for future treatments.
Fibrosis in Lymph Nodes and Immune Failure
Another striking finding was the extensive fibrosis - or scarring - in the mediastinal lymph nodes. These nodes, responsible for coordinating immune responses, showed a loss of structure and functionality. Histological analyses revealed excess collagen and fibroblast infiltration, which disrupted lymphocyte activity. This structural collapse weakens the immune system, leaving the body unable to mount an effective defense against the virus.
Interestingly, the patterns of lymph node damage correlated with markers of RAAS overactivation, suggesting a direct link between these phenomena. This insight helps explain why some COVID-19 patients suffer prolonged immune suppression, even months after infection.
Implications for Long COVID
The study's findings extend beyond immediate mortality. Researchers observed that chronic RAAS activation might underlie some symptoms of long COVID, such as fatigue, brain fog, and persistent inflammation. The fibrosis and immune dysregulation in lymph nodes could also explain why some patients develop chronic health issues post-infection.
Therapeutic Opportunities and Future Directions
Targeting RAAS overactivation offers a promising path for treatment. Drugs that inhibit RAAS components, such as ACE inhibitors or bradykinin antagonists, may help manage severe COVID-19. Additionally, interventions aimed at restoring mitochondrial health could mitigate immune overactivation and improve patient outcomes.
The study also highlights the need for early interventions to prevent the progression to severe disease. Strategies like early use of anti-inflammatory medications and close monitoring of immune markers could make a significant difference.
Concluding Insights
The study underscores the complexity of severe COVID-19, where multiple pathways converge to produce devastating outcomes. By focusing on RAAS overactivation, mitochondrial dysfunction, and lymph node fibrosis, researchers have provided a clearer picture of the disease's systemic effects. These findings hold promise for developing targeted therapies and improving survival rates in critically ill patients.
In summary, severe COVID-19 is not merely a respiratory illness; it is a systemic disease with far-reaching impacts. Understanding its underlying mechanisms is crucial for combating its most devastating effects.
The study findings were published in the peer-reviewed journal: PNAS.
https://www.pnas.org/doi/epub/10.1073/pnas.2401968121
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/statins-and-raasi-drugs-linked-to-lower-il-6-levels-in-covid-19-patients
https://www.thailandmedical.news/news/breaking-ace2-university-of-cincinnati-study-proves-china-s-research-wrong-on-virus-ace2-binding-effects-on-renin-angiotensin-aldosterone-system-raas