The Immune System's Role in Myocarditis - Unraveling Complex Pathways for Better Therapies
Nikhil Prasad Fact checked by:Thailand Medical News Team May 27, 2024 10 months, 4 weeks, 2 days, 12 hours, 30 minutes ago
Medical News: Myocarditis, an inflammatory disease affecting the heart muscle, presents a diagnostic challenge due to its heterogeneous nature. Defined as an inflammatory condition of the myocardium, it can manifest through various clinical presentations and etiologies. The 2013 consensus document from the European Society of Cardiology (ESC) Working Group on Myocardial and Pericardial Diseases offers a detailed and updated definition of myocarditis. This definition emphasizes specific histological, immunohistochemical, and immunological criteria to standardize diagnosis and address the longstanding challenges in disease classification. A study review by researchers from University of Padova-Italy that is covered in this
Medical News report uncovers the immune system’s role in Myocarditis.
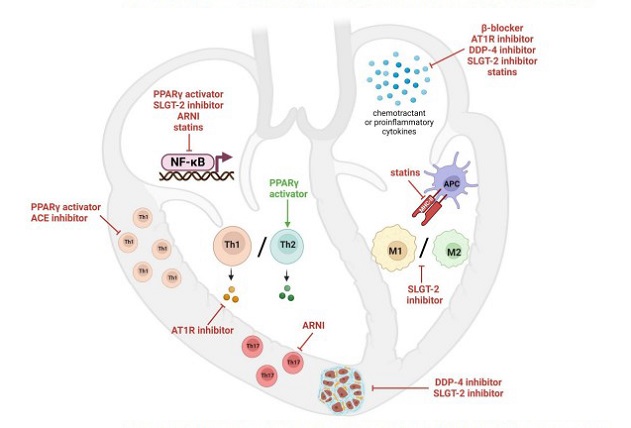
 Immunomodulatory effects of repurposed drugs in myocarditis. The figure shows the main pathogenetic mechanisms in myocarditis that are targeted not only by classical immunosuppressive agents, but also by other drugs with a different primary mechanism of action. (PPAR = Peroxisome Proliferator Activated Receptor; SGLT-2 = Sodium/Glucose Cotransporter 2; ARNI = Angiotensin receptor-neprilysin inhibitors; ACE = Angiotensin converting enzyme; AT1R = Angiotensin-II Receptor 1; DDP-4 = Dipeptidyl Peptidase 4; NF-κB = nuclear factor kappa-lightchain-enhancer of activated B cells; Th = T helper lymphocyte; M = macrophage; MHC-II = Major histocompatibility complex class II; APC = antigen presenting cell).
Historical Context and Diagnostic Evolution
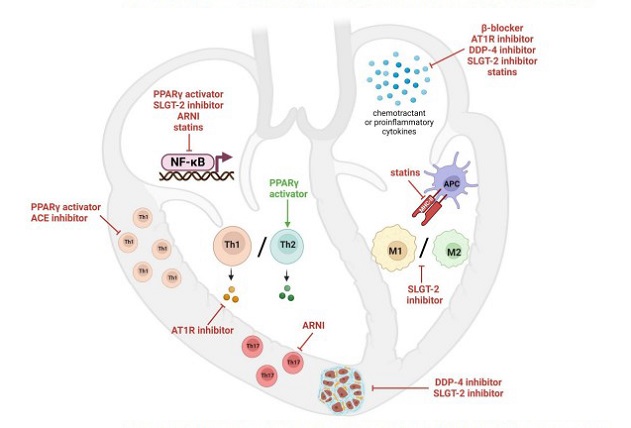
Immunomodulatory effects of repurposed drugs in myocarditis. The figure shows the main pathogenetic mechanisms in myocarditis that are targeted not only by classical immunosuppressive agents, but also by other drugs with a different primary mechanism of action. (PPAR = Peroxisome Proliferator Activated Receptor; SGLT-2 = Sodium/Glucose Cotransporter 2; ARNI = Angiotensin receptor-neprilysin inhibitors; ACE = Angiotensin converting enzyme; AT1R = Angiotensin-II Receptor 1; DDP-4 = Dipeptidyl Peptidase 4; NF-κB = nuclear factor kappa-lightchain-enhancer of activated B cells; Th = T helper lymphocyte; M = macrophage; MHC-II = Major histocompatibility complex class II; APC = antigen presenting cell).
Historical Context and Diagnostic Evolution
The term "myocarditis" was first coined in 1837 by French pathologist Jean Cruveilhier, who noted inflammation and necrosis in the hearts of individuals who succumbed to rheumatic fever. However, a modern understanding began to take shape only in 1982, when Woodroof JF et al. proposed an etiopathogenetic classification system. Advances in endomyocardial biopsy (EMB) techniques and cardiovascular pathology have been pivotal in identifying inflammatory cell infiltration in the myocardium.
The 2013 ESC consensus introduced quantitative criteria for pathological characterization, including the presence of specific leukocyte and T-lymphocyte counts in EMB samples. This was a significant advancement over the 1995 WHO classification, which lacked established quantitative criteria, leading to diagnostic heterogeneity. Immunohistochemistry (IHC) has also emerged as a critical technique for identifying and phenotyping inflammatory infiltrates in EMB, enhancing the accuracy of myocarditis diagnosis.
Clinical Presentation and Challenges
Diagnosing myocarditis remains complex due to its variable clinical presentation. Symptoms can range from acute chest pain to chronic heart failure, unexplained ventricular arrhythmias, or cardiogenic shock. Cardiac magnetic resonance (CMR) has become a pivotal non-invasive diagnostic tool, offering detailed myocardial tissue characterization. The updated Lak
e Louise criteria require evidence of both myocardial edema and non-ischemic myocardial injury to suspect inflammation, though these criteria need further validation in larger patient cohorts.
Etiology: Infectious and Non-Infectious Myocarditis
The etiology of myocarditis is diverse, with both infectious and non-infectious causes. Viral infections are the most common, with enteroviruses, adenoviruses, Parvovirus B19, and Human Herpesvirus 6 being notable culprits. Bacterial and parasitic infections, such as Chagas disease in Central and South America, also contribute. In viral myocarditis, the damage may arise from direct viral replication or immune responses triggered by molecular mimicry between viral antigens and myocardial proteins.
Non-infectious myocarditis, often immune-mediated, can be isolated or part of systemic immune-mediated diseases (SIDs). A significant recent concern is immune checkpoint inhibitor-related myocarditis (ICIM), which, though rare, can be severe and potentially fatal.
Immunopathological Processes in Myocarditis
Myocarditis pathogenesis involves both innate and adaptive immunity across three phases: acute, subacute, and chronic. In the acute phase, innate immunity responds to infection with cytokine and chemokine release, recruiting inflammatory cells to the heart. Monocytes and macrophages play a pivotal role, with M1 macrophages promoting inflammation and M2 macrophages aiding in tissue repair.
The adaptive immune response dominates the subacute phase, involving T helper cells (Th1, Th2, Th17) and regulatory T cells (Treg). Th1 cells, through cytokines like IL-12 and IFN-γ, mediate early tissue damage but also regulate excessive inflammation. Th2 cells and associated cytokines contribute to eosinophilic myocarditis. Th17 cells, driven by IL-6 and IL-23, are crucial for myocarditis progression, particularly in transitioning to heart failure.
Therapeutic Approaches: Targeting Immune Pathways
Immunosuppressive therapy (IT) is recommended for select cases of histologically confirmed virus-negative myocarditis, particularly severe forms like giant cell myocarditis (GCM) and cardiac sarcoidosis. Evidence supports IT's efficacy in improving left ventricular function and overall survival in virus-negative lymphocytic myocarditis, though viral presence in the myocardium contraindicates its use.
Combination therapy with corticosteroids and agents like Azathioprine (AZA) or Mycophenolate Mofetil (MMF) is standard for lymphocytic myocarditis, while more aggressive regimens are required for GCM. Novel therapeutic approaches, including monoclonal antibodies targeting specific immune pathways, show promise in managing myocarditis. Mepolizumab, an anti-IL-5 antibody, and Rituximab, an anti-CD20 antibody, have shown efficacy in treating eosinophilic myocarditis and selected cases of virus-negative myocarditis, respectively.
Repurposing Traditional Drugs for Myocarditis
Recent research has explored the immunomodulatory potential of traditional drugs not originally designed for myocarditis treatment. β-adrenergic receptor blockers like carvedilol, and Angiotensin-II receptor antagonists (sartans) such as losartan, demonstrate cardioprotective and anti-inflammatory effects in myocarditis models.
Anti-diabetic drugs like Pioglitazone, a PPAR-γ activator, show promise by inhibiting pro-inflammatory pathways. Sodium/glucose cotransporter 2 (SGLT-2) inhibitors (gliflozins) also exhibit anti-inflammatory properties, reducing fibrosis and cardiac inflammation.
Conclusion: Future Directions
The complex immunopathology of myocarditis requires continued research to fully understand and effectively target its various pathways. Current guidelines advocate for a combination of immunosuppressive and optimal medical therapy tailored to individual patient profiles. Emerging evidence suggests that traditional heart failure medications may have additional immunomodulatory benefits, paving the way for innovative therapeutic strategies. Further clinical studies are essential to explore these possibilities and improve outcomes for myocarditis patients.
The study review was published in the peer reviewed journal: Biomedicines.
https://www.mdpi.com/2227-9059/12/6/1156
For more about Myocarditis, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/rna-m5c-modification-plays-a-key-role-in-sars-cov-2-induced-myocarditis
https://www.thailandmedical.news/news/breaking-hong-kong-study-finds-that-covid-19-mrna-vaccines-activates-cd57-nk-cells-that-leads-to-acute-myocarditis
https://www.thailandmedical.news/news/viral-infections-can-lead-to-arrhythmias-and-cardiac-deaths-in-early-stages-of-infections-even-before-myocarditis-sets-in