The Lack Of Data On Musculoskeletal Involvement After Mild to Moderate COVID-19 Infection
Nikhil Prasad Fact checked by:Thailand Medical News May 10, 2024 11 months, 2 weeks, 2 days, 21 hours, 51 minutes ago
COVID-19 News: The outbreak of COVID-19 caused by the novel coronavirus SARS-CoV-2 has had a profound impact on global health and economies since its emergence in 2020. While much attention has been given to severe cases requiring hospitalization, there remains a significant gap in our understanding of the musculoskeletal effects of COVID-19 on individuals with mild to moderate forms of the disease who were not hospitalized. This study review covered in this
COVID-19 News report by researchers from Federal University of São Carlos (UFSCar)-Brazil aims to delve into the current knowledge and gaps in research regarding the musculoskeletal system in COVID-19, emphasizing the importance of studying mild to moderate cases and the need for more experimental data in this area.
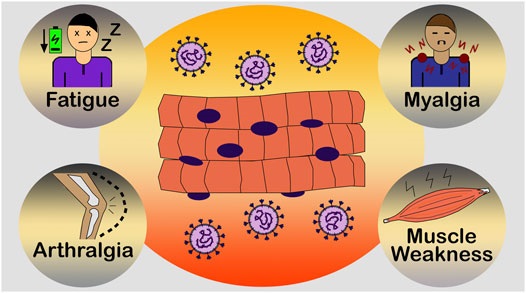
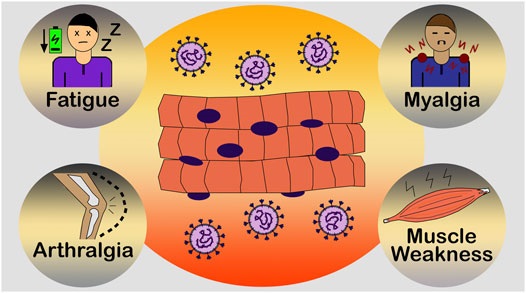 Lack Of Data On Musculoskeletal Involvement After Mild to Moderate COVID-19 Infection. Common muscle symptoms of COVID-19. Fatigue, arthralgia (joint pain), myalgia (muscle pain) and muscle weakness have been reported as initial and common symptoms by SARS-CoV-2-positive individuals. These extenuating symptoms can affect the daily lives of numerous individuals, reducing their quality of life.
Susceptibility of Skeletal Muscle Cells to SARS-CoV-2 Infection
Lack Of Data On Musculoskeletal Involvement After Mild to Moderate COVID-19 Infection. Common muscle symptoms of COVID-19. Fatigue, arthralgia (joint pain), myalgia (muscle pain) and muscle weakness have been reported as initial and common symptoms by SARS-CoV-2-positive individuals. These extenuating symptoms can affect the daily lives of numerous individuals, reducing their quality of life.
Susceptibility of Skeletal Muscle Cells to SARS-CoV-2 Infection
The human skeletal muscle, constituting a substantial portion of body weight, serves critical functions in movement, energy storage, and temperature regulation. Given its importance and the multisystemic nature of COVID-19, investigating the susceptibility of skeletal muscle to SARS-CoV-2 infection is crucial.
Two main hypotheses exist regarding the mechanism of action of the virus on skeletal muscle. The first proposes direct infection via the ACE2 receptor, although recent studies suggest an ACE2-independent interaction facilitated by TMPRSS2. The second hypothesis suggests an indirect mechanism through the inflammatory response, particularly the cytokine storm, which can lead to muscle fiber proteolysis and interfere with protein synthesis, contributing to fatigue and myalgia.
Furthermore, studies also suggest that pre-existing neuromuscular disorders may exacerbate musculoskeletal symptoms in COVID-19 patients. Conditions such as myasthenia gravis, motor neuron diseases, and myositis may be aggravated by viral infection or cytokine release, highlighting the complexity of musculoskeletal manifestations in COVID-19.
The Musculoskeletal Symptomatology
Musculoskeletal symptoms such as fatigue, arthralgia, myalgia, and muscle weakness are common in COVID-19 patients, often persisting after the acute phase of the infection. These symptoms can significantly impact daily activities and quality of life, especially in long-haulers or individuals with long-COVID.
Rhabdomyolysis, a severe skeletal muscle injury characterized by elevated levels of creatine kinase (CK) and myoglobin, has been reported in COVID-19 patients and can lead to acute kidney injury. The diverse rang
e of symptoms in COVID-19 makes prognosis challenging, necessitating a deeper understanding of the musculoskeletal manifestations and their diagnostic markers.
Furthermore, the different and somewhat discrepant symptoms of COVID-19, including the musculoskeletal ones, difficult the prognostic of the disease, and SARS-CoV-2 viral infection versus musculoskeletal symptomatology is still a subject poorly investigated and a challenge to the researchers in the Muscle Physiology field.
Long-COVID and Musculoskeletal Sequelae
Long-COVID refers to persistent symptoms lasting beyond the acute phase of COVID-19, affecting various organ systems, including the musculoskeletal system. Fatigue, myalgia, and joint pain are prevalent in long-haulers, and these symptoms can persist for months after the infection.
Risk factors for long-COVID include age, gender, comorbidities, reduced physical activity, and functional status. Understanding these sequelae is crucial for designing effective rehabilitation programs and providing appropriate care to long-hauler individuals.
Recent studies have suggested that the musculoskeletal symptoms, along with the neurological manifestations, prevail after the acute phase of infection, persisting for weeks and/or months, and giving rise to a debilitating condition named as long-COVID. While we are fighting COVID-19, numerous patients around the world, who have suffered from the disease, are calling themselves as “long-haulers,” that is, individuals who present post-COVID symptoms that are lasting even after recovery and viral elimination.
According to the guidelines of the National Institute for Health and Care Excellence (NICE) of the United Kingdom, long-COVID is defined as “signs and symptoms that continue after acute COVID-19, persisting for more than 4 weeks.
These long-term effects of COVID-19 are usually divided into two categories: (i) “continuous or ongoing symptomatic COVID-19,” which indicates symptoms lasting from 4 to 12 weeks; and (ii) “post-COVID-19 syndrome,” comprising signs and symptoms that persist beyond 12 weeks and are not elucidated by an alternative diagnosis except COVID-19.
Interestingly, while one past study reported that 60% of the individuals hospitalized for severe COVID-19 in a French cohort study complained of symptoms after 6 months of hospital admission, another study observed that even non-critical patients declare to have post-COVID symptoms.
https://www.sciencedirect.com/science/article/pii/S1198743X21001476
https://www.sciencedirect.com/science/article/pii/S1198743X20306066
This observation highlights the need of follow-up studies that include individuals who had mild to moderate COVID-19, and indicates that the post-COVID symptomatology (long-COVID) does not seem to occur only in people recovering from the severe and critical forms of the disease, as also observed by some reports.
Regarding the risk factors associated with long-COVID, they are not well defined; however, studies have reported that this condition occurs more in female patients and individuals with increased age and body mass index, presenting comorbidities, and with a reduced functional status and physical activity practice.
Additionally, the most prevalent symptoms in long-hauler individuals are fatigue, headache, dyspnea, and anosmia, which emphasizes a persistent neurological and musculoskeletal symptomatology as previously remarked. Fatigue is considered the musculoskeletal symptom most frequently reported by patients after recovery from COVID-19 while myalgias and arthralgias are also common complaints.
The Lack of Musculoskeletal Data Related to Mild to Moderate Forms of COVID-19
Despite the majority of COVID-19 cases being mild to moderate, research on the musculoskeletal effects in these individuals is scarce. Most studies focus on severe cases or long-term sequelae, leaving a gap in understanding the acute and long-term musculoskeletal manifestations in non-hospitalized patients.
Various types of studies have been conducted, including case reports, reviews, observational studies, and neurological assessments, but few delve into the specific musculoskeletal aspects of mild to moderate COVID-19. Functional tests, imaging techniques, and histological assays are underutilized in studying musculoskeletal symptoms in COVID-19.
Furthermore, some studies pointed out that the musculoskeletal symptomatology observed in COVID-19 positive patients can be due to pre-existing neuromuscular, muscular or autoimmune disorders, instead of symptoms directly caused by the viral infection. Three studies reported that individuals with myasthenia gravis, a chronic autoimmune disorder, had an exacerbation of their disease (mainly muscle weakness) after SARS-CoV-2 infection.
One study also suggested that individuals with motor neuron diseases and dystrophinopathies might be at elevated risk of manifesting exacerbating pre-existing muscle symptoms after COVID-19 infection. Lastly, myositis, a muscle inflammation that can induce muscle pain and weakness, symptoms observed in COVID-19, was well documented in numerous virus pathologies such as parainfluenza; influenza A/B; hepatitis A, B, C, and E; HIV; Dengue and West Nile, being considered a viral-related disease.
https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2021.607790/full
Although the association “myositis - COVID-19” has not yet been fully investigated, the increase in creatine kinase levels (aspartate aminotransferase (AST), alanine aminotransferase (ALT), and lactate dehydrogenase (LDH)) and myalgias, which are frequently observed in COVID-19 patients, suggest that the SARS-CoV-2 virus can induce an inflammatory myositis and contribute to muscle pain and weakness. Thus, these reports highlight that COVID-19 not only affects the muscle function by directly infecting muscle cells, but also can exacerbate pre-existing muscle disorders, suggesting a possible impact of the virus on the neuromuscular system.
Conclusion
In conclusion, the musculoskeletal involvement in mild to moderate COVID-19 cases remains underexplored despite its significant impact on patient well-being and quality of life. There is a critical need for more comprehensive research, including experimental data, imaging studies, and longitudinal assessments, to understand the mechanisms and long-term consequences of musculoskeletal manifestations in COVID-19 patients. This knowledge is essential for providing optimal care and support to individuals affected by COVID-19 across the spectrum of disease severity. The complex interaction between SARS-CoV-2 and the musculoskeletal system, along with the potential exacerbation of pre-existing neuromuscular disorders, underscores the importance of a multidisciplinary approach in managing COVID-19 patients and addressing their musculoskeletal symptoms. Future research should focus on elucidating the precise mechanisms of musculoskeletal involvement in COVID-19 and developing targeted interventions to improve patient outcomes and quality of life.
The study review was published in the peer reviewed journal:
https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2022.813924/full
For the latest
COVID-19 News, keep on logging to Thailand Medical News.
https://www.thailandmedical.news/news/musculoskeletal-and-neuropathic-pain-in-the-wake-of-the-covid-19-pandemic
https://www.thailandmedical.news/news/covid-19-news-scientists-warns-of-the-impact-of-sars-cov-2-on-the-musculoskeletal-system-and-calls-for-more-research
https://www.thailandmedical.news/news/brazilian-study-validates-that-covid-19-infections-also-affects-the-musculoskeletal-system