The neurobiological link between sleep, glymphatic dysfunction and neurodegeneration
Nikhil Prasad Fact checked by:Thailand Medical News Team Jul 22, 2024 1 year, 5 months, 3 weeks, 1 day, 3 hours, 45 minutes ago
Medical News: A new study highlights the critical role of sleep in maintaining brain health through a recently discovered system called the glymphatic system. This
Medical News report delves into the details of this fascinating research conducted by scientists from Vita-Salute San Raffaele University and IRCCS Istituto Policlinico San Donato in Milan, Italy, which explores how sleep impacts the brain's ability to clear neurotoxic proteins and the implications for neurodegenerative diseases.
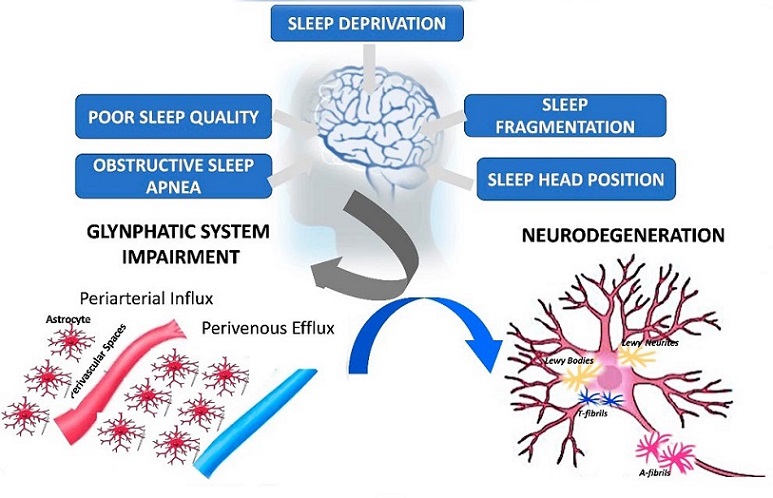
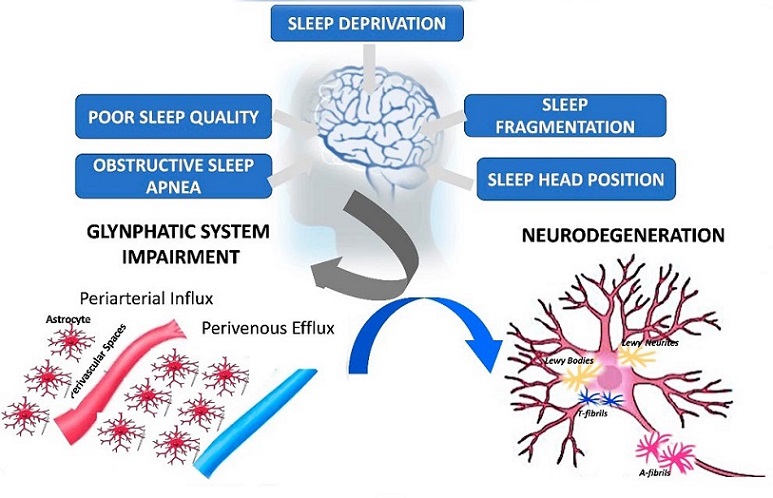 Schematic representation of the mechanisms linking sleep disorders, glymphatic system activity and neurodegeneration
Schematic representation of the mechanisms linking sleep disorders, glymphatic system activity and neurodegeneration
Understanding the Glymphatic System
In 2012, researchers identified the glymphatic system, a brain-wide network that facilitates the removal of metabolic waste from the brain. This system operates similarly to the lymphatic system in other parts of the body, but it is unique to the brain. The glymphatic system uses cerebrospinal fluid (CSF) to clear away waste products, including neurotoxic proteins like beta-amyloid, which are linked to conditions such as Alzheimer's disease.
The glymphatic system works in three main phases:
-CSF Inflow: CSF is produced in the choroid plexus and flows through periarterial spaces into the brain parenchyma.
-CSF-ISF Exchange: In the brain, CSF mixes with interstitial fluid (ISF) through a water channel protein called aquaporin-4 (AQP4), facilitating the exchange and movement of waste products.
-CSF Outflow: The mixed CSF-ISF drains out of the brain via perivenous spaces, eventually reaching systemic circulation and lymphatic systems.
Factors Influencing Glymphatic System Activity
The glymphatic system's efficiency is influenced by various factors, with sleep being the most significant. Research indicates that the glymphatic system is most active during sleep, particularly during non-rapid eye movement (NREM) sleep. During this phase, the interstitial space in the brain expands by 60%, enhancing the clearance of waste.
Other factors that affect the glymphatic system include:
-Head Position During Sleep: The supine position (lying on the back) may impede glymphatic activity due to the opening and closing of the jugular veins, which affects fluid dynamics.
-Cerebral Arterial Pulsatility: Arterial pulsations help drive the movement of CSF through the brain. Conditions that alter blood pressure or arterial pulsatility can impact glymphatic flow.
-Diet and Lifestyle: Omega-3 polyunsaturated fatty acids, moderate alcohol consumption, and physical activity can enhance glymphatic activity, while stress and hypertension can reduce it.
-Genetic Factors: Variants of the AQP4 gene, which
regulates water movement in the brain, can significantly influence glymphatic efficiency.
Glymphatic Dysfunction and Neurodegeneration
Neurodegenerative diseases like Alzheimer's and Parkinson's are characterized by the accumulation of misfolded proteins in the brain. The glymphatic system plays a crucial role in clearing these proteins, and dysfunction in this system can lead to their buildup, triggering a cascade of harmful effects.
Key Findings from the Study
The researchers found a strong link between glymphatic dysfunction and neurodegeneration. Key findings include:
-Sleep Disorders and Glymphatic Dysfunction: Poor sleep quality, sleep deprivation, and sleep fragmentation are associated with impaired glymphatic function. For example, obstructive sleep apnea (OSA) leads to increased venous pressure, reducing glymphatic clearance.
-Imaging Studies: Advanced neuroimaging techniques, such as diffusion tensor imaging (DTI) and MRI, have shown that glymphatic activity is reduced in patients with neurodegenerative diseases. The DTI-ALPS (Analysis Along the Perivascular Space) index, a measure of glymphatic function, correlates with cognitive performance and disease severity.
-Animal Models: Studies in mice have demonstrated that sleep deprivation impairs the clearance of waste products from the brain, supporting the idea that adequate sleep is essential for glymphatic function.
Implications for Treatment and Prevention
The findings suggest that targeting the glymphatic system could be a promising approach for treating and preventing neurodegenerative diseases. Strategies to enhance glymphatic function include improving sleep quality, managing blood pressure, and considering genetic factors related to AQP4.
Conclusion
The study underscores the importance of sleep in maintaining brain health and preventing neurodegeneration. By understanding and optimizing the factors that influence the glymphatic system, we can develop new interventions to protect the brain from the harmful effects of waste accumulation.
The study findings were published in the peer-reviewed journal: Clinical and Translational Neuroscience.
https://www.mdpi.com/2514-183X/8/2/23
For the latest on the Glymphatic System, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-causes-glymphatic-drainage-dysfunction-and-bbb-disruption-that-contributes-to-neuroaxonal-injury
https://www.thailandmedical.news/news/breaking-covid-19-news-study-alarmingly-finds-that-recovered-individuals-who-only-had-mild-covid-19-exhibit-glymphatic-system-dysfunction