U.S. NIH Study Finds That Removing Milk From Diets Helps With Treating Eosinophilic Esophagitis
Eosinophilic Esophagitis - Milk Mar 09, 2023 2 years, 1 month, 1 week, 4 days, 3 hours, 49 minutes ago
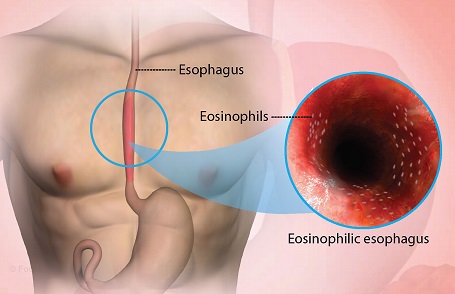
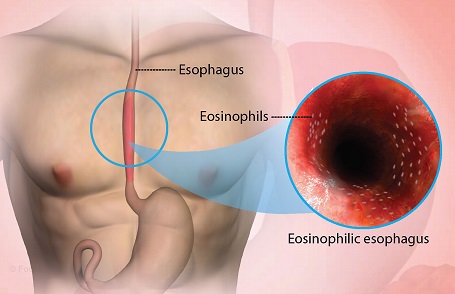
Eosinophilic Esophagitis (EoE) is a chronic disease characterized by an overabundance of white blood cells called eosinophils in the esophagus. Allergic inflammation due to food drives the disease by damaging the esophagus and preventing it from working properly. For individuals with EoE, swallowing even small amounts of food can be a painful and stressful choking experience. About 160,000 people in the United States are living with EoE.
The global prevalence of
Eosinophilic Esophagitis (EoE) has increased over the past 2 decades, nearly doubling in both adults and children, and occurring in an estimated one in 1,500 to 2,000 persons.
https://www.uspharmacist.com/article/prevalence-and-consequences-of-eosinophilic-esophagitis
Untreated Eosinophilic Esophagitis (EoE) may lead to permanent scarring or strictures and narrowing of the esophagus.
Excluding certain foods from the diet has been a cornerstone of EoE treatment.
During the early 2000s, researchers found that eliminating six common food triggers of esophageal injury—milk, egg, wheat, soy, fish, and nuts—substantially reduced signs and symptoms of EoE. This six-food elimination diet (6FED) became a common approach to managing the disease.
In recent years, scientists have conducted small, non-randomized studies of removing one to four of the most common food antigens from the diet to treat EoE, with some success. However, the relative risks and benefits of eliminating many foods versus a few foods at the start of diet-based therapy remained unclear.
This new clinical trial funded by theU.S. National Institutes of Health has found that eliminating just animal milk from the diet of adults with eosinophilic esophagitis (EoE) is as effective in treating the condition as eliminating animal milk and five other common foods.
The researchers noted that for individuals with EoE whose disease persists even after avoiding animal milk, a stricter diet may assist them in achieving remission.
These study findings were recently published in the peer reviewed journal: Gastroenterology & Hepatology.
https://www.thelancet.com/journals/langas/article/PIIS2468-1253(23)00012-2/fulltext
The new study findings come from the first multi-site, randomized trial comparing the 6FED (animal milk, wheat, egg, soy, fish and shellfish, and peanut and tree nuts) with a one-food elimination diet (1FED-animal milk) in adults with Eosinophilic Esophagitis (EoE). The trial was co-funded by NIAID, the National Center for Advancing Translational Sciences, and the National Institute of Diabetes and Digestive and Kidney Diseases, all part of NIH.
Dr Marc E. Rothenberg, M.D., Ph.D., the senior author of the published study, is director of both the Division of Allergy and Immunology and the Cincinnati Center for Eosinophilic Disorders at Cincinnati Children’s.
The
clinical trial involved 129 adults ages 18 to 60 years with a confirmed EoE diagnosis, active EoE symptoms, and a high number of eosinophils in esophageal tissue.
Volunteers enrolled in the trial at one of 10 U.S. medical centers that participate in the Consortium of Eosinophilic Gastrointestinal Disease Researchers, part of the NIH-funded Rare Diseases Clinical Research Network. Participants were assigned at random to either the 1FED, which eliminated only animal milk from the diet, or the 6FED.
The study participants followed their assigned diet for six weeks, then underwent an upper endoscopy exam and an esophageal tissue biopsy. If the number of eosinophils in the tissue indicated that EoE was in remission, the participant exited the study. If EoE was not in remission, individuals who had been on 1FED could advance to 6FED, and people who had been on 6FED could take topical swallowed steroids, both for six weeks, followed by a repeat exam with tissue biopsy.
The study findings showed that 34% of participants on 6FED and 40% of participants on 1FED achieved remission after six weeks of diet therapy, a difference that was not statistically significant. The two diets also had a similar impact across several other measures, including a reduction in EoE symptoms and an effect on quality of life.
Furthermore, the researchers discovered that almost half of the participants who did not respond to the one-food elimination diet (1FED) achieved remission after treatment with the more restrictive six-food elimination diet (6FED). In contrast, over 80% of the non-responders to 6FED achieved remission with oral steroids.
These study findings suggest that while 1FED is a reasonable first-line diet therapy option in adults with Eosinophilic Esophagitis (EoE), more restrictive diets may be necessary for some individuals to achieve remission. Additionally, for those who do not achieve remission with either 1FED or 6FED, oral steroids may be an effective treatment option.
Overall, these results offer hope for individuals with Eosinophilic Esophagitis (EoE) who struggle with the pain and discomfort of the condition. By identifying effective diet-based and medication-based therapies, healthcare providers can better manage EoE and improve the quality of life for those affected by the disease. Further research is needed to better understand the mechanisms behind Eosinophilic Esophagitis (EoE) and to develop more effective treatments.
For more on
Eosinophilic Esophagitis (EoE), keep on logging to Thailand Medical News.