UK Reports 66,730 Antibiotic-Resistant Infections in 2023. 2024 Set to Break Even More Alarming Records!
Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 17, 2024 4 months, 3 weeks, 5 days, 7 hours, 17 minutes ago
Medical News: The United Kingdom is grappling with an escalating health crisis as antibiotic-resistant infections hit an alarming 66,730 cases in 2023. This marked a significant rise from the 62,314 cases reported in 2019, surpassing pre-pandemic levels, according to the UK Health Security Agency (UKHSA). Preliminary data from 2024 suggests that the number of infections is on course to set an even higher record, underscoring the growing threat posed by antimicrobial resistance (AMR). This
Medical News report explores the implications of these findings and delves into what they mean for public health in the UK. It highlights the urgent need for coordinated action to tackle this silent yet devastating health emergency.
 UK Reports 66,730 Antibiotic-Resistant Infections in 2023. 2024 Set to Break Even More Alarming Records
UK Reports 66,730 Antibiotic-Resistant Infections in 2023. 2024 Set to Break Even More Alarming Records
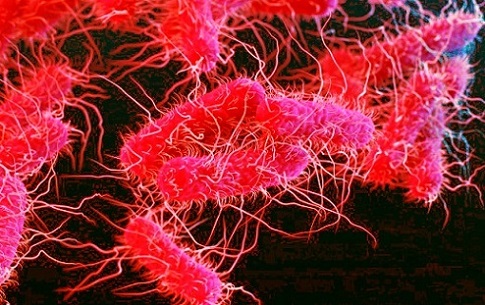
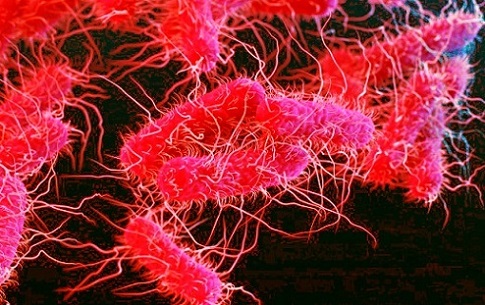
Image: Drug Resistant E.Coli Strains
Antibiotic-Resistant Infections on the Rise
Antibiotic-resistant infections occur when bacteria adapt and become immune to the effects of antibiotics, rendering standard treatments ineffective. This can lead to severe complications, including bloodstream infections, sepsis, prolonged hospital stays, and increased mortality rates. Individuals with antibiotic-resistant infections are more likely to die within 30 days than those with infections that respond to treatment.
The English Surveillance of Antibiotic Prescribing and Utilization Report (ESPAUR) attributes 65% of these infections over the past five years to Escherichia coli (E. coli).
https://www.gov.uk/government/publications/english-surveillance-programme-antimicrobial-utilisation-and-resistance-espaur-report
A common cause of urinary tract infections, diarrhea, and fever, E. coli has proven particularly resistant to antibiotics, driving the surge in serious bloodstream infections. Alarmingly, resistance to multiple antibiotic classes is also rising in pathogens like Klebsiella pneumoniae, further compounding the issue.
Impact on Vulnerable Communities
Data from 2023 revealed troubling disparities among communities. Those living in England's most deprived areas were 42.6% more likely to contract antibiotic-resistant infections compared to residents in wealthier regions. This gap has widened significantly from 29.4% in 2019. Over the last four years, infection rates among economically disadvantaged groups increased by 9.5%, painting a stark picture of inequality in healthcare outcomes.
Ethnic minorities have also borne a disproportionate burden, with Asian or Asian British groups reporting the highest proportion of antibiotic-resistant infections at 39.4%. Meanwhile, white ethnic groups accounted for nearly 90% of total cases. These findings underscore the need for targeted public health interventions to bridge these gaps and protect at-risk populations.
Antibiotic Consum
ption: A Concerning Trend
The rise in antibiotic use is another red flag. In 2023, antibiotic prescriptions increased by 2.4% compared to the previous year, returning to levels seen in 2019. Penicillins were the most frequently prescribed antibiotics in both primary and secondary care settings.
Professor Dame Jenny Harries, Chief Executive of UKHSA, highlighted the consequences of overprescribing antibiotics, stating, “Increasingly, the first antibiotics that patients receive aren’t effective at tackling their infections. That’s not just an inconvenience - it means they are at greater risk of developing severe infections and sepsis.”
She urged the public to only take antibiotics when prescribed by a healthcare professional and to avoid sharing leftover medications with others. Vaccination uptake was also emphasized as a critical measure to prevent infections and reduce the need for antibiotics.
The Human Cost of AMR
The personal stories of those affected by antibiotic-resistant infections offer a sobering perspective. Caroline Sampson, a patient battling a chronic urinary tract infection for over eight years, shared how her life has been upended. “No form of antibiotics has successfully treated it,” she explained. “It has derailed my life in every possible way. I live with daily anxiety that the infection could develop into urosepsis.” Her experience underscores the devastating impact AMR can have on individuals and their families.
What Is Being Done?
The UK government and health authorities are ramping up efforts to combat antibiotic resistance. Earlier this year, the UK unveiled its AMR National Action Plan for 2024-2029, which includes a target to reduce antibiotic use in human populations by 5% from the 2019 baseline. Investments in innovative tools and technologies are also part of the strategy to develop long-term solutions.
Collaborations with organizations like the Medicines and Healthcare products Regulatory Agency (MHRA) are driving the development of novel therapeutics and interventions. Dr. Nicola Rose, Interim Executive Director of Science and Research at MHRA, emphasized the importance of cutting-edge approaches such as microbiome-based therapies, phage therapy, and bacterial vaccines. Improved detection and surveillance of antimicrobial resistance genes are also being explored to identify threats early and implement timely interventions.
A Global Health Emergency
The threat of AMR extends beyond national borders. Minister for Public Health and Prevention Andrew Gwynne stressed the importance of international cooperation, particularly in light of commitments made at this year’s United Nations General Assembly. “This is an urgent global threat,” he said. “It is clear this emergency cannot be tackled by one nation alone.”
Global leaders are now recognizing AMR as a pressing issue, comparable in scale to the climate crisis. Collaborative efforts will be critical to funding research, standardizing quality benchmarks for therapeutics, and ensuring equitable access to treatments worldwide.
Conclusion
The rising tide of antibiotic-resistant infections in the UK is a stark reminder of the challenges ahead. With cases surpassing pre-pandemic levels and showing no signs of slowing, the consequences are grave - especially for the most vulnerable in society. From addressing health inequalities to advancing medical innovation, the fight against AMR demands a united front from policymakers, healthcare providers, and the public alike.
This is not a distant problem for future generations; it is an immediate crisis that threatens global health and economic stability. Simple steps, such as taking antibiotics responsibly, getting vaccinated, and supporting research into new treatments, can make a significant difference. The time to act is now to safeguard our ability to treat infections effectively in the years to come.
For the latest on antimicrobial resistance infections, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/herbs-and-phytochemicals-the-flavone-patuletin-from-marigold-is-able-to-inhibit-antibiotic-resistant-staphylococcus-aureus
https://www.thailandmedical.news/news/cannabis-study-shows-that-cannabidiol-cdb-could-help-in-fight-against-antibiotic-resistant-bacteria
https://www.thailandmedical.news/news/probiotic-drinks-to-combat-antibiotic-resistance