Understanding how COVID-19 affects T cells and macrophages especially in severe cases
Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 16, 2024 1 year, 4 months, 1 week, 5 days, 18 hours, 54 minutes ago
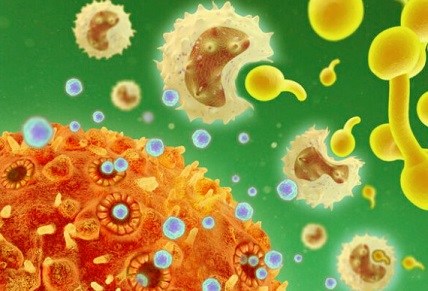
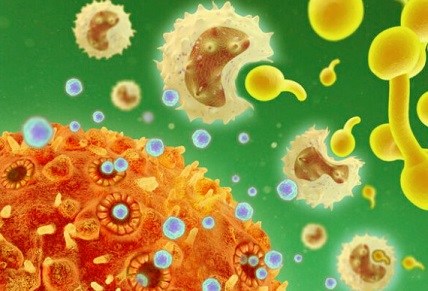
Medical News: A new study sheds light on how severe COVID-19 affects the immune system, with a focus on the roles of T cells and macrophages. Researchers from the State Key Laboratory of Respiratory Disease and the First Affiliated Hospital of Guangzhou Medical University, along with teams from the Guangzhou National Laboratory in China, investigated how immune cells react in cases of severe COVID-19. This
Medical News report explores their findings and the potential implications for treatment.
 Understanding how COVID-19 affects T cells and macrophages especially in
Understanding how COVID-19 affects T cells and macrophages especially in
severe cases
The researchers analyzed immune cells from severe COVID-19 patients, particularly focusing on pleural effusion, sputum, and peripheral blood samples. They found that severe cases of the disease led to significant immune dysfunction, especially in T cells and macrophages.
Key Findings From The Study
One of the main discoveries of this research is the exhaustion of T cells, which are crucial in fighting infections. The researchers noted that in patients with severe COVID-19, T cells become overactivated, leading to a state of exhaustion. This exhaustion reduces their ability to fight off the virus effectively.
Macrophages, another type of immune cell, were also found to play a significant role in severe COVID-19. The study identified a group of macrophages, known as M2 macrophages, that are involved in immune suppression. These M2 macrophages were abundant in patients with severe COVID-19 and may contribute to the exhaustion of T cells.
The research highlighted that the presence of these macrophages and exhausted T cells was particularly pronounced in the pleural fluid of patients, which surrounds the lungs. This indicates that the immune dysregulation in severe COVID-19 is more concentrated in the lung area, which is consistent with the severe respiratory symptoms seen in these patients.
How the Study Was Conducted
The study involved collecting samples from the pleural effusion, sputum, and peripheral blood of severe and mild COVID-19 patients. Single-cell RNA sequencing was used to analyze the immune cells present in these samples. This technique allowed the researchers to observe how different types of immune cells responded to the virus.
They discovered that while most immune cells were present in both mild and severe cases, there were significant differences in the activation levels of these cells. In severe cases, T cells were found to be highly activated, but this overactivation led to their exhaustion. The macrophages in these patients also showed signs of being in a pro-inflammatory state, further contributing to immune dysregulation.
The Role of Transposable Elements
Another fascinating aspect of the study was the examination of transposable elements (TEs), which are small pieces of DNA that can move around within the genome. The researchers found that in severe COVID-19 patients, there was a significant increase in the activity of certain
TEs, particularly in macrophages. This increased activity may play a role in the immune dysfunction observed in these patients.
While TEs have been known to regulate immune responses in other diseases, this is one of the first studies to suggest that they may also be involved in the immune response to COVID-19. The researchers believe that the increased activity of TEs could be contributing to the exhaustion of T cells and the activation of macrophages in severe COVID-19 cases.
Why T Cells and Macrophages Are Important in COVID-19
T cells are a crucial part of the immune system, helping to identify and destroy infected cells. In most viral infections, including COVID-19, T cells play a vital role in controlling the spread of the virus. However, in severe cases of COVID-19, the overactivation and subsequent exhaustion of T cells make it difficult for the body to mount an effective immune response.
Macrophages, on the other hand, are responsible for engulfing and destroying pathogens. They also play a role in regulating the immune response by releasing signals that either activate or suppress other immune cells. In the case of severe COVID-19, the researchers found that M2 macrophages were particularly abundant. These macrophages are known for their anti-inflammatory properties, but in this context, they may be contributing to the suppression of T cells, preventing them from effectively fighting the virus.
Potential Implications for Treatment
The findings of this study could have significant implications for the treatment of severe COVID-19. The discovery that M2 macrophages are contributing to T cell exhaustion suggests that targeting these macrophages could be a potential therapeutic strategy.
One possibility is to develop treatments that reduce the activity of M2 macrophages, allowing T cells to function more effectively. Another approach could be to find ways to boost T cell activity, helping them to overcome exhaustion and fight off the virus more effectively.
The study also suggests that monitoring pleural effusion could provide valuable insights into the immune response of COVID-19 patients. By analyzing the immune cells present in pleural fluid, doctors may be able to get a better understanding of how the immune system is responding to the virus and tailor treatments accordingly.
Conclusion
This study provides new insights into how severe COVID-19 affects the immune system, particularly focusing on the roles of T cells and macrophages. The discovery that M2 macrophages contribute to T cell exhaustion could lead to new therapeutic strategies aimed at improving immune function in patients with severe COVID-19.
The researchers also highlighted the potential role of transposable elements in immune dysregulation, suggesting that these small pieces of DNA could be involved in the immune response to COVID-19.
As the world continues to battle the COVID-19 pandemic, studies like this are crucial for understanding how the virus affects the immune system and for developing more effective treatments for those who are most severely affected by the disease.
The study findings were published in the peer-reviewed journal: Heliyon.
https://www.cell.com/heliyon/fulltext/S2405-8440(24)14719-6
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/french-study-finds-that-sars-cov-2-infection-in-the-lungs-primarily-targets-specific-pulmonary-macrophages
https://www.thailandmedical.news/news/macrophages-drive-inflammation-and-symptoms-in-sars-cov-2-infected-gut