Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 08, 2024 1 year, 2 months, 1 hour, 33 minutes ago
Medical News: The Virus Behind Many Lymphomas
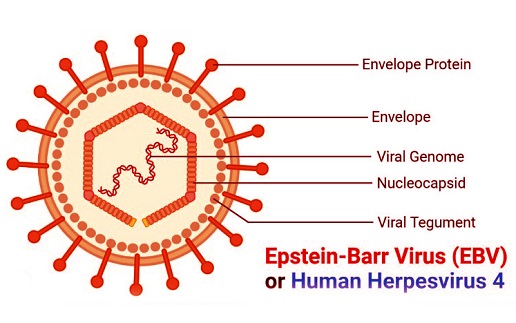
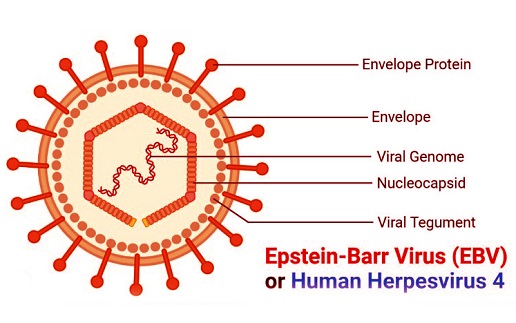
Epstein-Barr Virus (EBV) is a common virus infecting more than 90% of adults worldwide, yet only a small percentage develop cancer from it. Researchers, including Ya-Fang Chiu from Chang Gung University in Taiwan, Khongpon Ponlachantra from the Vidyasirimedhi Institute of Science and Technology in Thailand, and Bill Sugden from the University of Wisconsin-Madison, aim to understand how this virus sometimes leads to serious diseases like lymphoma. This
Medical News report delves into how EBV operates within our cells and why it can lead to cancer in some cases.
 Understanding How Epstein-Barr Virus Leads to Different Types of Lymphomas
Key Findings: Types of Lymphomas Linked to EBV
Understanding How Epstein-Barr Virus Leads to Different Types of Lymphomas
Key Findings: Types of Lymphomas Linked to EBV
EBV is linked to five main types of lymphomas: Burkitt lymphoma, NK/T cell lymphoma, Hodgkin’s lymphoma, Diffuse Large B Cell Lymphoma (DLBCL), and Primary Effusion Lymphoma (PEL). The frequency of EBV-positive lymphomas varies based on geographical location and type. For example, more than 90% of Burkitt lymphoma cases in Central Africa are EBV-positive, while in the United States, only about 29% show EBV presence. This virus is also found in nearly all cases of nasal NK/T cell lymphoma globally, while only 40% of Hodgkin’s lymphoma cases are EBV-positive.
Though EBV infects a vast majority of the population, only a rare few develop lymphoma due to it. The virus drives lymphoma formation through its presence in cancer cells, which may promote the survival and growth of these cells. This is evident from studies indicating EBV’s presence as circular plasmids in cancer cells, which are retained only if they provide an advantage to those cells. Some lymphomas even exhibit integrated EBV DNA, which embeds directly into the host cell’s DNA. These occurrences raise the question of why only some individuals progress to cancer.
Factors Behind EBV-Induced Lymphomas
Several key factors influence whether an EBV infection progresses to lymphoma. Researchers have outlined three main contributing factors: rare EBV variants, human genetic susceptibility, and co-infections.
-EBV Variants and Their Role
Scientists have been examining whether specific strains of EBV are more likely to lead to lymphoma. However, while there are geographical clusters of certain EBV variants, no specific EBV strain has been conclusively linked to higher cancer rates. For instance, a study comparing EBV strains from Guatemala and Southeast Asia found that these variants were more geographically than disease-specific.
-Genetic Vulnerability
Genetic predisposition also plays a role in determining who might be susceptible to EBV-induced lymphomas. Certain genetic mutations can impair the body’s ability to manage EBV. For example, people with mutations in the SH2D1A gene, linked to a condition known as Duncan’s syndrome, face a higher risk of developing EBV-related lymphomas. Similarly, mutations affecting magnesium tran
sport, which hampers immune cell function, can also increase lymphoma risk. Such genetic factors point to a crucial interplay between EBV infection and the body’s immune capabilities.
-Co-Infections That Complicate EBV’s Role
The presence of other infections, especially malaria and HIV, can enhance EBV’s ability to induce lymphomas. Malaria, for instance, increases the number of EBV-infected cells, which may explain the higher prevalence of Burkitt lymphoma in malaria-endemic regions. On the other hand, HIV’s impact on the immune system further compromises the body’s ability to keep EBV in check, leading to a significantly higher risk of EBV-positive lymphomas in individuals with HIV. This synergy between infections emphasizes the need for comprehensive management in areas where such diseases coexist.
EBV’s Oncogenic Mechanisms: How It Triggers Lymphomas
EBV drives lymphoma formation through three main mechanisms: promoting cell proliferation, preventing cell death, and suppressing immune recognition.
-EBV’s Influence on Cell Growth
EBV’s EBNA2 protein promotes the uncontrolled growth of B cells by interacting with proteins that trigger cell proliferation. EBNA2 activates numerous genes, including c-Myc, a common oncogene, thus facilitating cell proliferation.
Meanwhile, another EBV protein, LMP1, mimics signals from immune cells to keep infected cells alive and multiplying, laying the groundwork for tumor formation.
-Blocking Cell Death
EBV prevents the programmed cell death (apoptosis) of infected cells. EBV’s EBNA3 proteins, for example, block the production of a protein called Bim, which is crucial for initiating cell death. In this way, EBV ensures that infected cells persist, further increasing the risk of cancerous growth. Additionally, the viral gene LMP2A provides signals to infected B cells, helping them avoid apoptosis even in the absence of essential cellular signals. By keeping infected cells alive, EBV creates a conducive environment for lymphoma development.
-Escaping Immune Surveillance
EBV has mechanisms to evade the immune system, allowing infected cells to evade detection. EBNA1, the viral protein responsible for maintaining the EBV genome within cells, effectively hides from immune surveillance. EBNA1 limits its own presentation to immune cells, minimizing the chances of detection. Similarly, EBV miRNAs interfere with immune processes, allowing infected cells to evade recognition by the body’s defenses.
Rare Cancers Despite High Infection Rates
Despite EBV’s high infection rate, lymphomas caused by this virus remain rare. Researchers believe that a combination of factors, including EBV’s ability to stay latent and the immune system’s capability to control it, keeps cancer risk low. EBV infection usually remains dormant in memory B cells, where it expresses minimal or no viral proteins. This latency means that the virus is often invisible to the immune system, thus avoiding any reaction. In cases where the virus reactivates, usually due to immune system failure or additional factors, it may lead to uncontrolled cell growth and lymphoma.
Conclusion
The Epstein-Barr Virus is a widespread but mostly silent player in human health. While it infects most people at some point, only a fraction will ever develop EBV-related lymphomas. This rarity is thanks to EBV’s complex relationship with the immune system and its ability to remain hidden in cells. However, in certain cases, like co-infections or genetic vulnerabilities, the virus can disrupt cellular processes and lead to cancer. Understanding EBV’s mechanisms gives researchers insight into developing therapies that could potentially interrupt its cancer-causing pathways, offering hope for those at risk.
The study findings were published in the peer-reviewed journal: Viruses.
https://www.mdpi.com/1999-4915/16/11/1744
For the latest on the Epstein-Barr Virus, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/reactivation-of-herpesviruses-like-epstein-barr-virus-and-cytomegalovirus-could-be-causing-long-covid-issues
https://www.thailandmedical.news/news/study-links-human-papilloma-virus-epstein-barr-virus-and-cytomegalovirus-with-breast-cancer
https://www.thailandmedical.news/news/herbs-and-phytochemicals-french-study-shows-that-shikonin,-an-inhibitor-of-inflammasomes-can-also-inhibit-epstein-barr-virus-reactivation
https://www.thailandmedical.news/news/epstein-barr-virus-cancer-study-finds-that-epstein-barr-virus-contributes-to-the-oncogenesis-of-mature-t-cell-lymphoproliferative-neoplasms
https://www.thailandmedical.news/news/new-study-shows-that-epstein-barr-virus-reactivation-and-low-cortisol-levels-are-common-in-many-long-covid-patients