Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 04, 2024 5 months, 1 week, 2 days, 3 hours, 2 minutes ago
Medical News:
What is Painful Legs and Moving Toes Syndrome?
Painful Legs and Moving Toes (PLMT) syndrome is a rare neurological disorder that causes chronic pain and involuntary toe movements. Described as an uncommon movement disorder, PLMT combines two troubling symptoms - persistent leg pain and involuntary toe movements. The pain typically feels deep within the legs and is often accompanied by repetitive, seemingly uncontrollable movements of the toes, which can intensify with certain movements or positions. This
Medical News report delves into a recent case study that sheds light on this poorly understood condition.
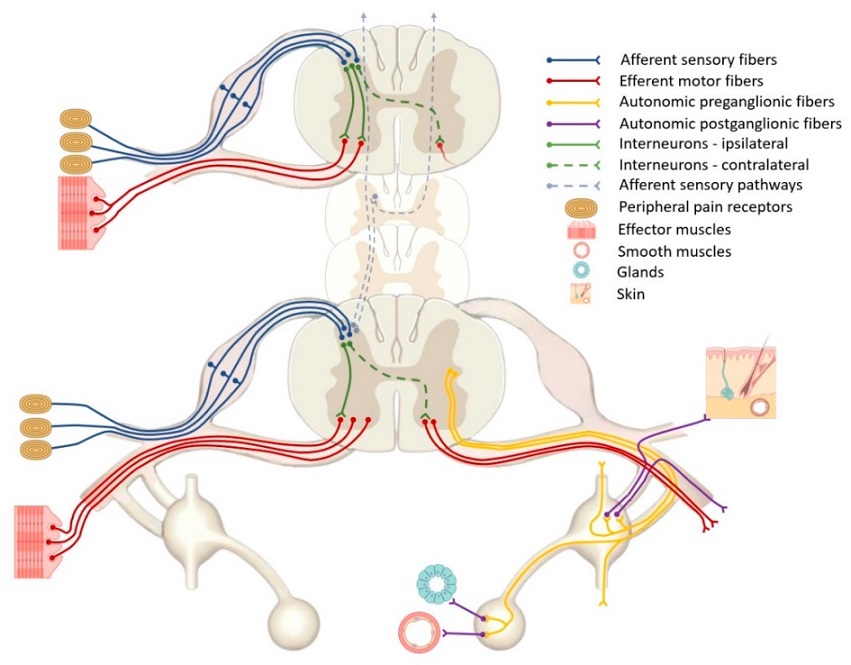
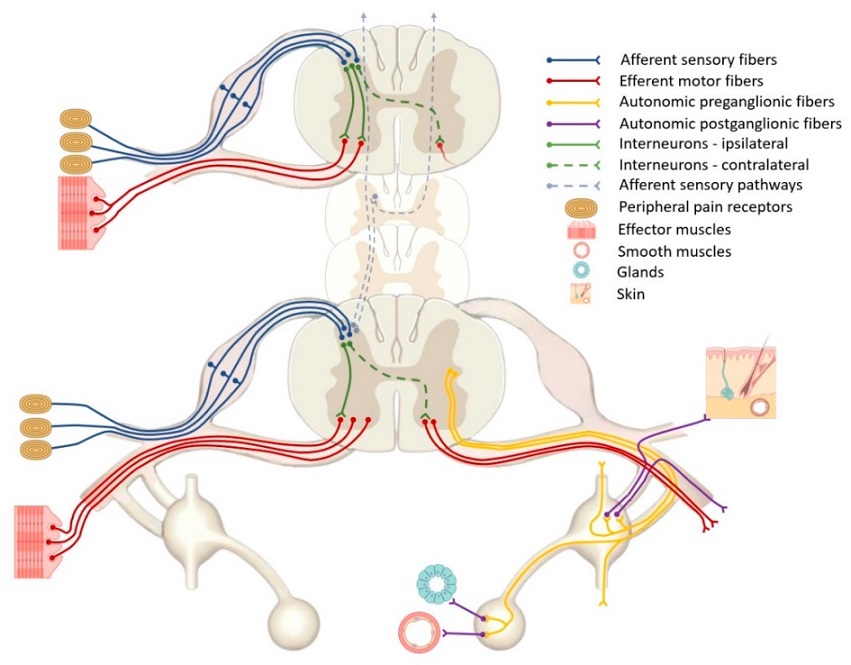 Leading pathogenetic mechanisms of painful legs and moving toes syndrome (PLMT)—role of interneurons, autonomic fibers, and remote trigger points.
A Rare Case Study
Leading pathogenetic mechanisms of painful legs and moving toes syndrome (PLMT)—role of interneurons, autonomic fibers, and remote trigger points.
A Rare Case Study
In a recent case, a 49-year-old man reported to the Second Clinic of Neurology at University Hospital “St. Marina” in Varna, Bulgaria. He had been struggling with pain radiating from his lower back to his thigh, which soon transformed into a more widespread discomfort that reached the toes on his right foot. Involuntary movements in his toes followed, adding to the daily challenge of managing his symptoms. Over-the-counter painkillers, anti-inflammatories, and B vitamins were no match for his symptoms.
When doctors examined the patient, they observed constant, involuntary movements in his right toes, worsened by physical stimulation to the right thigh. To determine the cause, the medical team conducted an MRI of his lumbar and cervical spine, uncovering several bulging discs and myelopathy, which is damage to the spinal cord, between the C5-C7 vertebrae. The team diagnosed him with PLMT due to discogenic issues and proposed treatment with Pregabalin, which brought significant symptom relief. The patient refused surgery but saw substantial improvement with the medication, reporting reduced pain and an eventual cessation of involuntary movements.
Exploring the Causes of PLMT
The origins of PLMT are still unclear. First identified in 1971 by neurologist John David Spillane, PLMT has long puzzled researchers. Over the years, various theories emerged, linking it with nerve damage, spinal cord injuries, peripheral neuropathy, or previous trauma. Researchers at the University Hospital “St. Marina” suggested that a combination of sensory and motor nerve disruptions could be involved, with abnormalities in the nervous system leading to involuntary muscle activity.
Some cases indicate that PLMT could originate in the peripheral nervous system, while others suggest central nervous system involvement. When damage to sensory pathways occurs, it disrupts regular nerve signal transmission. In PLMT patients, minor stimuli - like light touches or circular motions - can activate motor neurons, causing erratic toe movements.
Diagnosing PLMT: A Complex Process
Given its rarity, diagnosing PLMT often involves excluding other disorders with similar symptoms. Patients usually report
deep, neuropathic pain that can be stabbing, tingling, or electric. Involuntary movements in PLMT are distinct, appearing irregular, and in response to sensory stimulation, with symptoms intensifying at certain times of day. Doctors recommend EMG (electromyography) and MRI scans to assess nerve and spinal cord health.
For instance, in the Bulgarian case, an EMG showed reduced muscle action potential and slower nerve conduction, pointing to peripheral neuropathy. MRI scans are especially valuable, helping to identify bulging discs or structural anomalies that may compress nerves or the spinal cord, leading to PLMT symptoms.
Treatment: Addressing Both Pain and Movements
Treating PLMT presents challenges, as each patient may respond differently. While there is no definitive cure, doctors aim to manage pain and movement symptoms using a combination of medication and, in some cases, physical therapy or surgery. Here are some of the most common treatment options explored for PLMT:
Medications
-GABA Modulators: Drugs that influence GABA (gamma-aminobutyric acid) have been particularly effective in relieving PLMT symptoms. GABA is a neurotransmitter that inhibits nerve transmission, helping to reduce pain and control involuntary movements. For instance, Pregabalin, as seen in the case study, provided long-term relief without side effects.
-Antidepressants and Antipsychotics: Some antidepressants, antipsychotics, and anticonvulsants have shown temporary effectiveness, but results vary. Commonly used drugs include amitriptyline, propranolol, and quetiapine.
Non-Medication Options
-Botulinum Toxin Injections: Botulinum toxin injections have become a popular choice for controlling movement and reducing pain. By blocking nerve signals that cause muscle contraction, the treatment has shown effectiveness lasting several months, making it a practical choice for severe cases.
-Sympathetic Nerve Blockade: In some cases, doctors may recommend sympathetic nerve blockade, which interrupts pain signals by injecting anesthetics around the nerves. This method has been beneficial for some patients, but the effects are usually temporary.
Surgical and Device-Based Options
-Spinal Cord Stimulation (SCS): SCS involves implanting a small device near the spine that emits electrical pulses, interrupting pain signals before they reach the brain. SCS has shown promise in controlling both pain and movement symptoms, offering relief for up to a year after implantation.
-Sympathectomy and Decompression Surgery: Sympathectomy, or removing parts of the sympathetic nervous system, can be helpful, particularly if nerve compression is the cause of PLMT. Decompression surgery is another option for those with discogenic pathology, offering the possibility of long-term relief.
Key Findings and Insights from the Case Study
The patient in this case study experienced considerable improvement with Pregabalin, which is often used for neuropathic pain. This anticonvulsant was titrated to 300 mg daily, effectively reducing pain and halting involuntary toe movements. Over a follow-up period of 90 days, the patient reported minimal discomfort, with pain levels dropping to a manageable level. This case highlights Pregabalin’s potential as a first-line treatment option for PLMT, offering a non-invasive alternative to surgery.
Moreover, the involvement of tactile stimulation in this case suggests that PLMT symptoms might be linked to sensory nerve disruption, which creates an abnormal feedback loop, amplifying pain and movement. This insight could guide future research, prompting doctors to investigate sensory stimuli’s role in triggering or worsening symptoms.
Concluding Thoughts
Painful Legs and Moving Toes syndrome, though rare, can significantly impact a person’s quality of life. The condition’s roots appear to lie in a mix of peripheral and central nervous system disruptions, particularly where sensory and motor nerves intersect. This case study underscores the importance of early treatment, with drugs like Pregabalin providing substantial relief. Surgical and device-based treatments remain options for severe cases, especially when conservative treatments fail.
Ongoing research will be essential to deepen our understanding of PLMT. Physicians must remain vigilant in identifying symptoms and offering individualized treatment plans that address both pain and involuntary movements.
The study findings were published in the peer-reviewed journal: Neurological International.
https://www.mdpi.com/2035-8377/16/6/102
For the latest on Painful Legs and Moving Toes Syndrome, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/medical-updates-from-switzerland:-erythema-nodosum-what-you-need-to-know
https://www.thailandmedical.news/news/uk-doctors-warn-of-venous-insufficiency-and-acrocyanosis-blue-legs-in-long-covid