University Of Birmingham Study Finds That SARS-Cov-2 Infections Can Cause A Variety Of Immune-Mediated Inflammatory Diseases Including T1DM, IBD And Psoriasis!
Source: Long COVID Oct 12, 2022 3 years, 3 months, 1 week, 4 days, 10 hours, 48 minutes ago
A new study by researchers from University of Birmingham-UK has found that SARS-CoV-2 infections can also trigger a variety of immune-mediated inflammatory diseases (IMIDS) especially type 1 diabetes mellitus, inflammatory bowel disease (IBD) and psoriasis.
The aim of the study was to assess whether there is an association between SARS CoV-2 infection and the incidence of immune mediated inflammatory diseases (IMIDs).
The study involved a matched cohort study involving primary care electronic health record data from the Clinical Practice Research Datalink Aurum database.
The study cohort included 458,147 adults aged 18 years and older with a confirmed SARS CoV-2 infection by reverse transcriptase polymerase chain reaction (RT-PCR) or lateral flow antigen test, and no prior diagnosis of IMIDs.
The study participants were matched on age, sex, and general practice to 1,818,929 adults in the unexposed cohort with no diagnosis of confirmed or suspected SARS CoV-2 infection and no prior diagnosis of IMIDs.
The primary outcome measure was a composite of the incidence of any of the following IMIDs:
-autoimmune thyroiditis
-coeliac disease
-inflammatory bowel disease (IBD)
-myasthenia gravis
-pernicious anemia
-psoriasis
-rheumatoid arthritis (RA)
-Sjogren’s syndrome
-systemic lupus erythematosus (SLE)
-type 1 diabetes mellitus (T1DM)
-vitiligo
The secondary outcomes were the incidence of each of these conditions separately. Cox proportional hazards models were used to estimate adjusted hazard ratios (aHR) and 95% confidence intervals (CI) for the primary and secondary outcomes comparing the exposed to the unexposed cohorts, and adjusting for age, sex, ethnic group, smoking status, body mass index, relevant infections, and medications.
The study findings showed that 537 patients (0.11%) in the exposed cohort developed an IMID during the follow-up period over 0.29 person years, giving a crude incidence rate of 3.54 per 1000 person years. This was compared 1723 patients (0.09%) over 0.29 person years in the unexposed cohort, with an incidence rate of 2.82 per 1000 person years.
Patients in the exposed cohort had a 22% relative increased risk of developing an IMID, compared to the unexposed cohort (aHR 1.22, 95% CI 1.10 to 1.34).
The incidence of three IMIDs were statistically significantly associated with SARS CoV-2 infection. These were T1DM (aHR 1.56, 95% CI 1.09 to 2.23), IBD (1.52, 1.23 to 1.88), and psoriasis (1.23, 1.05 to 1.42).
The study team concluded that SARS CoV-2 was associated with an increased incidence of IMIDs including T1DM, IBD and psoriasis. Further research is needed to replicate these findings in other populations and to measure autoantibody profiles in cohorts of individuals with COVID-19, including Long COVID and matched controls.
The study findings were published on a preprint server and are currently being peer reviewed.
https://www.medrxiv.org/content/10.1101/2022.10.06.22280775v1
Based on previous studies, it is already known that a subsection of the population who tested positive for SARS Co
V-2 typically suffer from a post-Covid-19 condition known as
Long COVID.
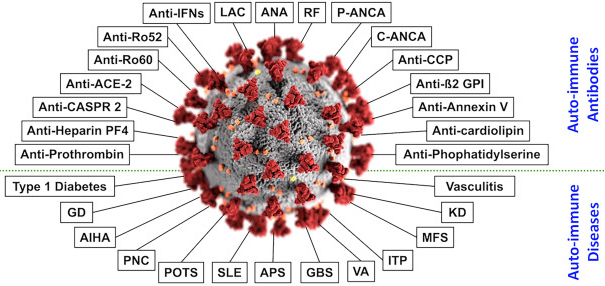
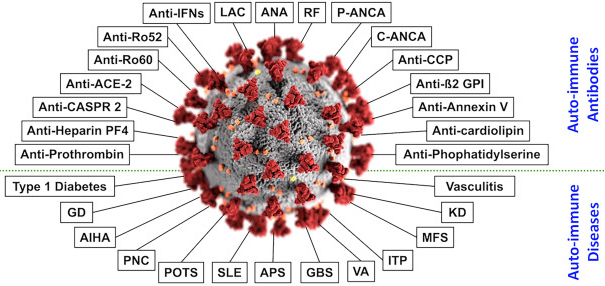
Numerous preliminary findings, such as case reports of post-COVID-19 IMIDs, increased autoantibodies in COVID-19 patients, and molecular mimicry of the SARS-CoV-2 virus have given rise to the theory that long COVID may be due in part to a deranged immune response.
This new study finding COVID-19 exposure was associated with a 22% relative increase in the risk of developing certain IMIDs, including type 1 diabetes mellitus, inflammatory bowel disease, and psoriasis.
The study findings provide further support to the hypothesis that a subgroup of Long Covid may be caused by immune mediated mechanisms.
To date, SARS-CoV-2 infections have caused the deaths of more than 6.56 million people globally according to reported figures. (Actual figures can be five or six-fold!)
More worryingly, it is estimated that more than 3 billion people around the world have already been exposed to the SARS-CoV-2 coronavirus. With studies showing that about 33 percent of this population expected to also suffer from
Long COVID, the burden on public healthcare, the economy and also society is phenomenally overwhelming.
Already, many individuals who have recovered from COVID-19 have reported the persistence of various symptoms. These symptoms comprise post-acute sequelae that are collectively referred to as ‘
Long COVID’. Despite over one-third of people with COVID-19 reporting persistent symptoms, the pathogenesis of this condition remains unclear.
The study team are among the first to explore the potential association between SARS-CoV-2 infection and immune-mediated inflammatory diseases (IMIDs).
Based on past studies, it has been theorized that SARS-CoV-2 infection causes an inappropriate immune response that is responsible for the symptoms of
Long COVID.
Importantly, a significant and persistent rise in autoantibodies in COVID-19 patients compared to uninfected controls has supported this theory. Case reports of patients experiencing dysfunctional immune manifestations have also been described in systematic reviews.
One past study showed that thyroid dysfunction was up to 20% of patients. This is linked to B- and T-cell autoimmunity, which could be driven by the homology between human and SARS-CoV-2 proteins, a phenomenon called molecular mimicry.
https://pubmed.ncbi.nlm.nih.gov/34024217/
Interestingly, the mechanisms responsible for IMIDs could also include molecular mimicry and system dysregulation during COVID-19. Alternatively, tissue damage and the release of autoantigens could also contribute to the pathogenesis of this condition.
To date, evidence supporting these hypotheses is based on small cohorts and case reports, both of which are not strong study designs for causal inference.
Furthermore, most data have been drawn from patients with moderate or severe disease, thus underrepresenting asymptomatic or mild cases, mainly associated with long COVID.
In order to address the aforementioned limitations, a retrospective matched cohort study was conducted using data from a major primary care database. The exposed cohort comprised 458,147 adults aged 18 years and older with confirmed SARS-CoV-2 infection and no prior diagnosis of IMIDs.
All these study patients were matched with 1,818,929 adults in the unexposed cohort based on age, sex, and general practice. Individuals in the unexposed cohort neither had a prior diagnosis of IMIDs nor confirmed or suspected SARS-CoV-2 infection.
The study findings showed that compared to the unexposed cohort, the exposed cohort was associated with a 22% relative increase in the incidence of the considered IMIDs during the same period.
More specifically, the association between SARS-CoV-2 infection and T1DM, inflammatory bowel disease, and psoriasis was particularly strong.
Significantly, individuals in the exposed cohort were 56%, 52%, and 23% more likely to develop T1DM, IBD, and psoriasis, respectively, as compared to the unexposed cohort. Notably, 40% of all new diagnoses across both cohorts were for IBD and psoriasis.
It was also found that age and sex were major risk factors associated with the incidence of IMIDs.
It was found that the likelihood of females being diagnosed with an IMID was 30% higher than males. Further, individuals aged 40-49 years and 50-59 years were less likely to be diagnosed with an IMID as compared to individuals aged 18-29 years.
Importantly, the large sample size of over two million provided sufficient statistical power to infer differences in the incidence of IMIDs across the two groups. Furthermore, important demographic and clinical risk factors were controlled. The study findings could also be generalized, as nationwide data were used.
Study limitations include missing data for ethnicity, body mass index (BMI), smoking status, and socioeconomic factors. Since community testing was not common during the first wave of the pandemic, there could be some misclassification across the two cohorts. Also, it is possible that only a fraction of IMID cases were detected during the short follow-up study period.
The study team stressed that since it has already been widely documented that SARS-CoV-2 infection is associated with many IMIDs, such as psoriasis, IBD, and T1DM, these suggest that
Long COVID might be partly related to elevated autoimmunity.
More detailed research is warranted on other diverse populations to confirm the current study findings.
For the latest
Long COVID-19 Research, keep on logging to Thailand
Medical News.