Unraveling The Mysteries Of Long COVID - A Comprehensive Analysis Of Neural Consequences Through Blood Markers
Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 09, 2024 1 year, 11 months, 2 days, 13 hours, 20 minutes ago
COVID-19 News: Long COVID-19 (LongC) has emerged as a perplexing and persistent health condition affecting millions worldwide. The aftermath of SARS-CoV-2 infection extends beyond the acute phase, giving rise to lingering symptoms collectively referred to as LongC. In a pioneering effort, the San Francisco VA Health Care System and the University of California, San Francisco, have conducted an extensive study, focusing on blood markers to explore the intricate neural consequences of LongC. This
COVID-19 News report, delves into the findings of this research, shedding light on the complexities of LongC and its impact on the nervous system.
 Neural Consequences of Long COVID Shown Via Blood Markers
Neural Consequences of Long COVID Shown Via Blood Markers
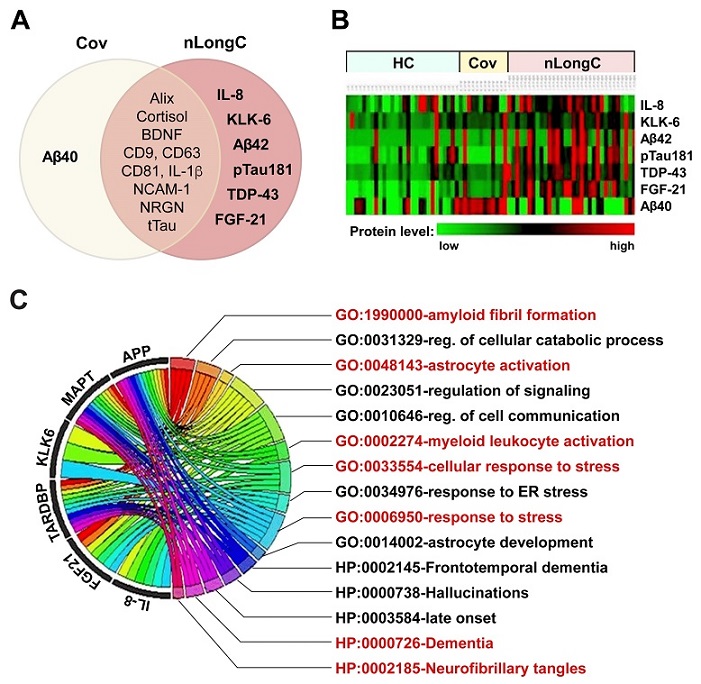
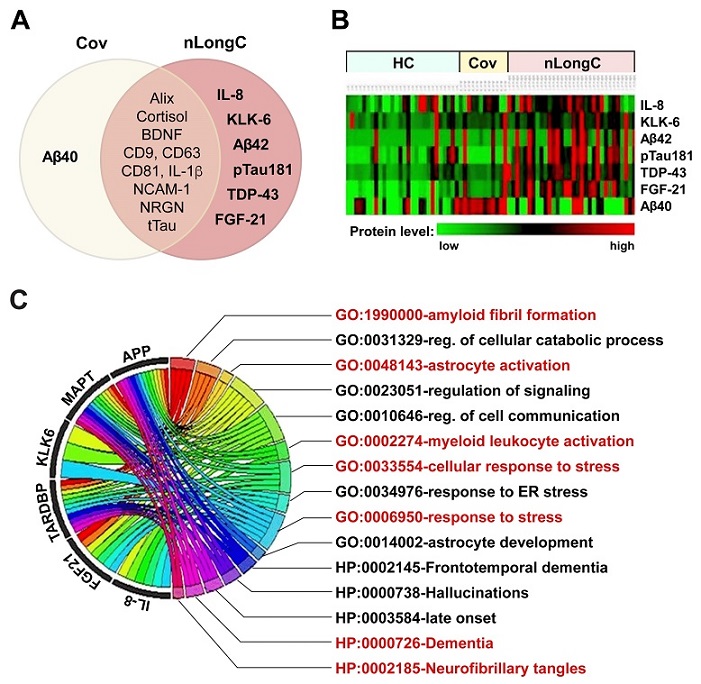
Blood biomolecules and informatics classification analyses for nLongC. (A) Venn diagram delineating the differentially expressed blood biomolecules identified in this study. (B) Heatmap of eight critical blood protein levels, with samples from healthy controls (HC) on the left, Cov in the middle, and nLongC on the right. Red represents higher expression and green represents lower expression. (C) Chord diagram depicting the connections between the genes and their associated GO and HP terms, providing insights into the biological processes and functions related to nLongC pathogenesis. GO and HP terms, along with their respective biological processes, indicated in red, represent potential pathological mechanisms of nLongC, some of which show associations to AD.
Long COVID: A Multifaceted Challenge
With over 65 million registered cases of LongC, this condition has become a significant health concern. LongC affects individuals of diverse ages and backgrounds, with an estimated incidence rate ranging from 10% to 70% for non-hospitalized and hospitalized cases, respectively. The severity of LongC is associated with the acute phase of the disease, and its prevalence is particularly notable in individuals aged 36 - 50, representing the majority of COVID-19 cases.
The neurological sequelae of LongC (nLongC) present a wide array of symptoms affecting both the peripheral and central nervous systems. Muscle weakness, cognitive impairment, sleep disorders, and various other neurological manifestations contribute to the complexity of LongC. Notably, 31% of LongC cases have no identified preexisting chronic comorbidities, and females are more likely than males to be diagnosed with LongC.
Addressing the Gaps in Long COVID Research
Despite the increasing prevalence of LongC, the lack of effective diagnostic tools and targeted treatments poses a significant challenge. The absence of a comprehensive understanding of the underlying mechanisms hinders progress in addressing the lingering symptoms observed in LongC patients. This research seeks to bridge these gaps by exploring blood markers, providing a unique perspective on the neural consequences of LongC.
Role of Extracellular Vesicles in Neural Health
Extracellular vesicles (EVs) have emerged as essential play
ers in understanding the physiological state of cells and their role in various diseases. Neuronal-enriched EVs (nEVs) offer a window into the health of the nervous system, as they carry molecular cargo reflective of the parent cell. These vesicles can cross the blood-brain barrier, making them valuable indicators of brain-related conditions.
In previous research, the investigative team utilized nEVs to analyze blood biomarkers in individuals with nLongC at a time point of 2–3 months post-infection. The findings indicated protein changes suggestive of peripheral cytokine reactions and differentially expressed neurodegenerative proteins. Building upon these insights, the current study extends the investigation to individuals with nLongC approximately one-year post-infection.
Insights from Blood Markers: A Detailed Analysis
The study involved 45 COVID-19 participants, classified into three groups: 33 with neurological symptoms (nLongC), 12 without lingering symptoms (Cov), and 28 pre-COVID-19 healthy controls (HC). A thorough analysis of blood markers provided crucial insights into the aftermath of COVID-19 infection.
-Plasma Cytokines: Peripheral markers of inflammation were assessed using a seven multiplex MSD cytokine array. The analysis revealed elevated levels of IL-1β in both nLongC and Cov groups, while IL-8 was specifically increased in nLongC. These cytokines suggest a chronic peripheral inflammation, indicative of a sustained immune response post-infection.
-Neurotrophic Factors and Stress: Brain-derived neurotrophic factor (BDNF) and cortisol, markers associated with synaptic plasticity and stress, exhibited significant elevation in both nLongC and Cov groups compared to healthy controls. The correlation between BDNF and IL-1β, coupled with the inverse relationship between BDNF and cortisol, implies ongoing inflammation and stress in LongC individuals.
-Extracellular Vesicle Characterization: nEVs from nLongC individuals displayed distinct characteristics, including larger sizes and higher concentrations compared to Cov and HC. Tetraspanins and exosome marker Alix were elevated in nEVs from nLongC, indicating altered cargo reflective of neuronal dysfunction.
-Neurodegenerative Proteins: A panel of neurodegenerative proteins was identified as significantly upregulated in nEVs from nLongC individuals, including Aβ42, pTau181, and TDP-43. These proteins are associated with conditions like Alzheimer's disease (AD), hinting at a potential link between LongC and neurodegenerative processes.
-Informatic Analysis: Bioinformatics tools were employed to unravel the functional significance of the identified markers. The analysis highlighted associations with AD-related terms, emphasizing potential links between LongC and accelerated AD development or progression. Additionally, terms related to stress and myeloid cell activation pointed towards underlying pathophysiological aspects of LongC.
Discussion and Limitations
Despite the study's limitations, including a relatively small sample size, lack of cognitive testing standardization, and absence of participants with pre-existing cognitive impairment, the findings provide a compelling rationale for further exploration. The observed differences in blood markers between healthy controls, recovered individuals, and those with neurological symptoms underscore the need for larger longitudinal studies.
Conclusion
This groundbreaking study offers unprecedented insights into the neural consequences of LongC through a comprehensive analysis of blood markers. The chronic peripheral inflammation, altered stress response, and distinctive neurodegenerative protein profiles identified in nEVs provide a foundation for understanding the lingering impact of COVID-19 on the nervous system. As the scientific community continues to unravel the complexities of LongC, this research paves the way for future investigations, aiming to guide diagnostic and therapeutic strategies for this enigmatic condition. The study not only deepens our understanding of LongC but also opens avenues for potential biomarkers and treatment modalities to address the persistent neurological symptoms associated with this condition.
The study findings were published in the peer reviewed journal: Cells.
https://www.mdpi.com/2073-4409/13/6/478
For the latest
COVID-19 News, keep on logging to Thailand Medical News.