Unveiling the role of Helicobacter pylori in exacerbating COVID-19 gastrointestinal symptoms
Sebastian Lavoie Fact checked by:Thailand Medical News Team Sep 06, 2024 7 months, 2 weeks, 6 days, 5 hours, 42 minutes ago
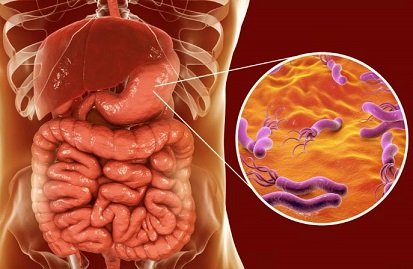
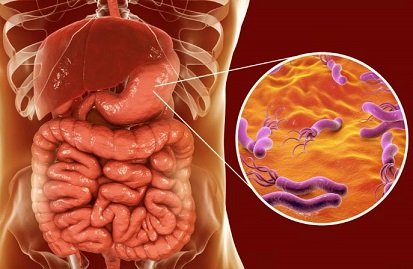
Medical News: Recent research has shed new light on how the co-infection of Helicobacter pylori (H. pylori), a common bacterial pathogen, and SARS-CoV-2, the virus responsible for COVID-19, exacerbates gastrointestinal symptoms in patients. This
Medical News report explores the intricate relationship between these two infections and provides insights into their combined impact on the gut, potentially opening new avenues for treatment and management.
 Unveiling the role of Helicobacter pylori in exacerbating COVID-19 gastrointestinal symptoms
Unveiling the role of Helicobacter pylori in exacerbating COVID-19 gastrointestinal symptoms
The study was conducted by researchers from the Indian Institute of Technology Indore, the Central Ayurveda Research Institute in Kolkata, the School of Biotechnology at Devi Ahilya Vishwavidyalaya, and the Regional Ayurveda Research Institute in Gwalior. Their findings could pave the way for better understanding the severity of COVID-19 in patients with pre-existing H. pylori infections.
Co-Infection and Its Consequences
H. pylori, a bacterium present in over 50% of the global population, is primarily known for its role in causing gastritis, peptic ulcers, and even gastric cancer. While not typically life-threatening, H. pylori's persistence in the gut can lead to chronic inflammation and weaken the gut's defenses. On the other hand, SARS-CoV-2, though primarily a respiratory virus, has been linked to a variety of gastrointestinal symptoms such as diarrhea, nausea, and abdominal pain.
The study explores how the co-infection of these two pathogens affects gut health. The study, conducted on colon carcinoma cells (HT-29), revealed that the co-infection of SARS-CoV-2 and H. pylori resulted in significantly elevated inflammation compared to the individual infections. The researchers found that inflammatory markers such as TNF-α, IL-6, and CXCL1 were highly upregulated in co-infected cells, indicating a heightened immune response.
The Mechanism Behind Co-Infection
The research delved deep into the molecular mechanisms of co-infection. Both H. pylori and SARS-CoV-2 are capable of activating the NF-κB pathway, a critical mediator of inflammation. In this study, the co-infected cells showed significantly higher levels of NF-κB activation compared to those infected by either H. pylori or SARS-CoV-2 alone. The presence of H. pylori appears to create a more favorable environment for SARS-CoV-2 to infect the gastrointestinal cells.
Further investigations revealed that co-infection led to a higher expression of β-catenin and c-Myc proteins, both of which are linked to cellular inflammation and cancer progression. This finding suggests that individuals with H. pylori infections might be more susceptible to severe gastrointestinal symptoms when infected with SARS-CoV-2.
Mitochondrial Dysfunction and Cell Death
One of the most alarming findings of the study was the damage to the mitochondria in co-infected cells. Mitochondria are the energy powerhouses of the cell, and any dysfu
nction in them can lead to severe cellular consequences. The study found that co-infection resulted in mitochondrial dysfunction, which contributed to necroptotic cell death - a form of programmed cell death associated with inflammation.
In contrast to apoptosis, which is a more controlled form of cell death, necroptosis triggers the release of inflammatory molecules, exacerbating tissue damage. The study showed that co-infected cells experienced higher levels of necroptosis, which could explain the severe gastrointestinal symptoms observed in some COVID-19 patients.
The researchers used markers such as RIPK1, a key regulator of necroptosis, to confirm the type of cell death occurring in the co-infected cells. They found that RIPK1 was significantly upregulated in the co-infection model, further supporting the hypothesis that necroptosis is a primary driver of cell death in these cases. This discovery adds another layer of complexity to our understanding of how SARS-CoV-2 interacts with other pathogens in the body.
Timing of Infection Matters
An interesting aspect of the study was the timing of the infections. The researchers found that pre-existing H. pylori infections led to more severe outcomes when followed by SARS-CoV-2 infection. This suggests that individuals already infected with H. pylori might be more vulnerable to severe COVID-19 symptoms, particularly in the gastrointestinal tract.
Conversely, the study also explored what happens when SARS-CoV-2 infects first, followed by H. pylori. While still harmful, the effects were not as pronounced as when H. pylori was present before the viral infection. This finding could have significant implications for how we approach treatment and prevention in populations with high rates of H. pylori infection.
Implications for Treatment
Understanding the interaction between H. pylori and SARS-CoV-2 could lead to new treatment strategies. For example, targeting the NF-κB pathway or inhibiting RIPK1 might help reduce inflammation and prevent necroptosis in co-infected individuals. Additionally, early detection and treatment of H. pylori infections could potentially reduce the severity of COVID-19 in high-risk populations.
The study also highlights the importance of personalized treatment plans. For patients with chronic H. pylori infections, addressing the bacterial infection before or during a SARS-CoV-2 infection could mitigate some of the more severe gastrointestinal symptoms. This is especially important in regions where H. pylori infection rates are high.
Conclusion: A Closer Look at the Gut's Role in COVID-19
This research underscores the importance of the gastrointestinal system in COVID-19 pathology. While SARS-CoV-2 is primarily a respiratory virus, its ability to infect the gut, particularly in the presence of other pathogens like H. pylori, suggests that more attention should be given to gastrointestinal symptoms in COVID-19 patients.
The study findings provide valuable insights into the molecular mechanisms of co-infection, highlighting the role of inflammatory pathways, mitochondrial dysfunction, and necroptotic cell death. As the global fight against COVID-19 continues, understanding these complex interactions will be crucial for developing more effective treatments and improving patient outcomes.
The study findings were published on a preprint server.
https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4853611
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/hong-kong-study-finds-that-new-omicron-variants-ba-2-86-and-jn-1-shift-from-airway-to-intestinal-tropism
https://www.thailandmedical.news/news/miami-study-sounds-alarm-that-mpox-can-also-cause-gastrointestinal-complications-and-inflammation-of-the-rectum