Warning! SARS-CoV-2 Infections Can Trigger And Accelerate Progression Of Creutzfeldt-Jakob Disease In Those With E200K Mutation!
Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 27, 2024 1 year, 4 weeks, 18 hours, 48 minutes ago
COVID-19 News: In recent times, the medical community has witnessed a concerning trend wherein patients infected with SARS-CoV-2, the virus responsible for COVID-19, have shown an increased risk of developing neurodegenerative diseases. Among these diseases is Creutzfeldt-Jakob Disease (CJD), a fatal neurodegenerative condition caused by prions that affect the central nervous system (CNS). This
COVID-19 News report delves into a specific case reported in Italy, highlighting the potential link between SARS-CoV-2 infection and the acceleration of CJD progression, especially in individuals with a genetic predisposition.
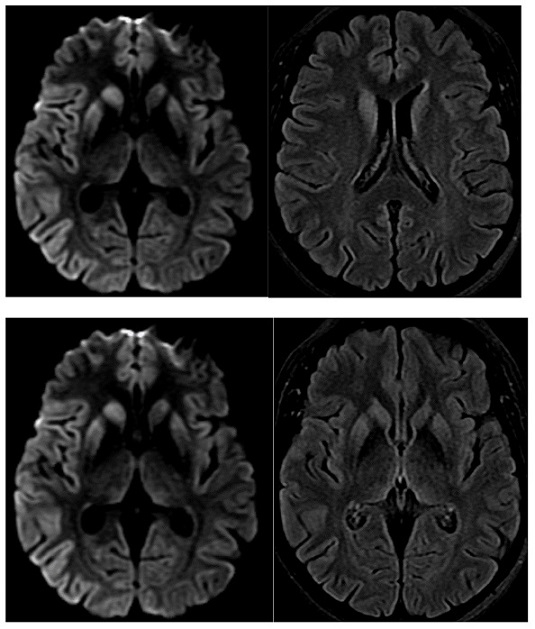
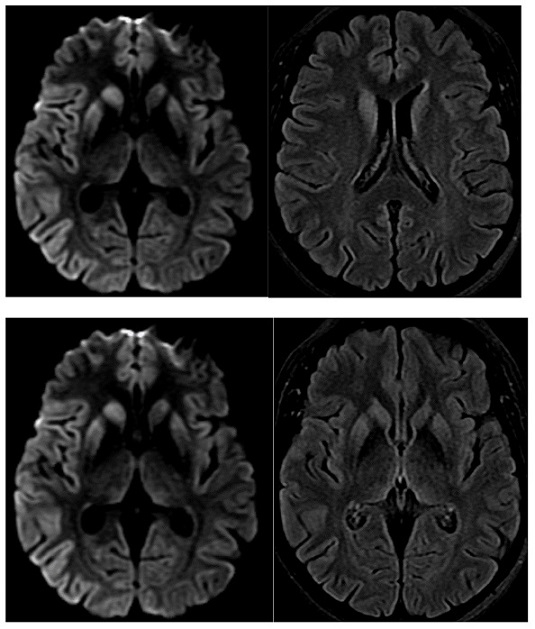 SARS-CoV-2 Infections Can Trigger And Accelerate Progression Of Creutzfeldt-Jakob Disease In Those With E200K Mutation. DWI, diffusion-weighted imaging abnormalities, typically reported in CJD in the cortical and basal ganglia.
Background: The Intersection of COVID-19 and Neurodegenerative Diseases
SARS-CoV-2 Infections Can Trigger And Accelerate Progression Of Creutzfeldt-Jakob Disease In Those With E200K Mutation. DWI, diffusion-weighted imaging abnormalities, typically reported in CJD in the cortical and basal ganglia.
Background: The Intersection of COVID-19 and Neurodegenerative Diseases
As the COVID-19 pandemic swept across the globe, Italy stood as one of the first European countries to face its formidable impact. The disease manifested in various clinical forms, ranging from mild symptoms to severe respiratory complications and multi-organ involvement. While vaccination efforts have mitigated the acute morbidity and mortality associated with COVID-19, attention has shifted towards understanding its long-term effects, particularly on neurological health.
Creutzfeldt-Jakob Disease (CJD): An Overview
CJD belongs to a group of neurodegenerative disorders known as transmissible spongiform encephalopathies (TSEs), characterized by the abnormal accumulation of prion proteins in the brain. Italy, like many other countries, has been actively monitoring and studying CJD cases to enhance diagnostic accuracy and treatment strategies. The identification of genetic mutations associated with CJD, such as the E200K mutation, has provided valuable insights into the disease's pathogenesis and clinical variability.
Case Study: Unraveling the Connection
Researchers from Sapienza University-Italy and San Camillo-Forlanini Hospital-Italy presented a case study involving a 51-year-old woman with a family history of CJD who developed symptoms of rapidly progressing dementia two months after a mild SARS-CoV-2 infection. Extensive clinical evaluations, including imaging studies, electroencephalography (EEG), and cerebrospinal fluid analysis, confirmed the diagnosis of CJD with the E200K mutation. This case is particularly significant as it underscores the potential role of SARS-CoV-2 infection in triggering and exacerbating CJD, especially in individuals with specific genetic mutations.
Clinical Findings and Genetic Analysis
The patient's clinical course, marked by cognitive decline and neurological abnormalities, aligns with classical CJD symptoms. Ge
netic testing revealed the E200K mutation with homozygosity for methionine (MET) at codon 129, further confirming the diagnosis. MRI findings demonstrated characteristic changes in brain regions typically affected in CJD, reinforcing the genetic association observed in similar cases.
Exploring the Mechanisms: SARS-CoV-2 and Neurodegeneration
The discussion delves into the potential mechanisms underlying the interaction between SARS-CoV-2 infection and neurodegenerative diseases like CJD. Studies suggest that the virus's neurotropic nature and systemic inflammatory responses may contribute to the acceleration of neurodegeneration. The activation of astrocytes and microglia, coupled with cytokine dysregulation, creates an environment conducive to protein misfolding and aggregation, hallmarks of prion diseases.
Genetic Variability and Clinical Phenotypes
CJD exhibits significant clinical heterogeneity, influenced by genetic factors such as the mutation at codon 129. Variations in clinical presentation and disease progression highlight the complexity of CJD and the importance of genetic counseling and testing, especially in familial cases. Insights from genetic analysis not only aid in diagnosis but also hold promise for future targeted therapeutic interventions.
Implications for Research and Clinical Practice
The article emphasizes the need for continued research to elucidate the intricate relationship between SARS-CoV-2 infection and neurodegenerative diseases. Understanding the molecular pathways and immune responses involved can guide the development of preventive measures and therapeutic strategies. Clinicians are encouraged to consider neurodegenerative complications in COVID-19 survivors, particularly those with genetic predispositions.
Conclusion: Navigating the Nexus of Infectious Diseases and Neurological Health
In conclusion, the reported case of CJD following SARS-CoV-2 infection underscores the complex interplay between infectious agents and neurodegenerative processes. While further investigation is warranted, this case serves as a poignant reminder of the multifaceted challenges faced in modern healthcare. By bridging the gaps between genetics, infectious diseases, and neurology, we can strive towards better outcomes for patients and enhanced preparedness for future health crises.
The case study and study findings were published in the peer reviewed journal: Clinical and Translational Neuroscience.
https://www.mdpi.com/2514-183X/8/2/16
For the latest
COVID-19 News, keep on logging to Thailand Medical News.