WARNING! Two New Studies Find That All Exposed To SARS-CoV-2 Are At High Risk Of Developing Heart Issues Up To A Year Or Longer After Infection!
Source: COVID-Cardiovascular Issues - Medical-News Feb 08, 2022 3 years, 10 months, 3 weeks, 2 days, 4 hours, 49 minutes ago
COVID-Cardiovascular Issues: Two new studies are providing evidence that all individuals who have been exposed to the SARS-CoV-2 coronavirus are at greater risk of developing a wide range of cardiovascular issues ranging from heart failures, cerebrovascular disorders, dysrhythmias, inflammatory disease of the heart or pericardium, ischemic heart disease, non-ischemic cardiomyopathy cardiac arrest, cardiogenic shock and even thromboembolic disorders, irrespective of if they were asymptomatic or had mild to severe conditions upon initial infection with the virus.
 Both studies showed the persistence of cardiovascular issues as one of the important manifestations of long COVID and the importance of regular heart health screenings for all those who had been exposed to the SARS-CoV-2 virus.
Both studies showed the persistence of cardiovascular issues as one of the important manifestations of long COVID and the importance of regular heart health screenings for all those who had been exposed to the SARS-CoV-2 virus.
In the first study by researchers from Washington University School of Medicine in St. Louis-USA, Saint Louis University-Missouri-USA and the Veterans Affairs St. Louis Health Care System-USA,
it was found that COVID-19 patients are at high risk of developing heart problems up to a year r more after infection with the SARS-CoV-2 virus, irrespective if they had mild symptoms or were hospitalized.
The
COVID-Cardiovascular Issues study team used the national healthcare databases from the US Department of Veterans Affairs to build a cohort of 153,760 individuals with COVID-19, as well as two sets of control cohorts with 5,637,647 (contemporary controls) and 5,859,411 (historical controls) individuals, to estimate risks and 1-year burdens of a set of pre-specified incident cardiovascular outcomes.
The study findings showed that beyond the first 30 days after SARS-CoV-2 infection, individuals with COVID-19 are at increased risk of incident cardiovascular disease spanning several categories, including cerebrovascular disorders, dysrhythmias, ischemic and non-ischemic heart disease, pericarditis, myocarditis, heart failure and thromboembolic disease.
Alarmingly these risks and burdens were evident even among individuals who were not hospitalized during the acute phase of the infection and increased in a graded fashion according to the care setting during the acute phase (non-hospitalized, hospitalized and admitted to intensive care).
The study findings provide evidence that the risk and 1-year burden of cardiovascular disease in survivors of acute COVID-19 are substantial. Care pathways of those surviving the acute episode of COVID-19 should include attention to cardiovascular health and disease.
The study findings were published in the peer reviewed journal: Nature Medicine.
https://www.nature.com/articles/s41591-022-01689-3
The detailed analysis of the federal health data confirmed that individuals who have had COVID-19 are at increased risk of developing cardiovascular complications within the first month to a year after infection. Such complications include disruptive heart rhythms, inflammation of the heart, blood clots, stroke, coronary artery disease, heart attack, heart failure or even death.
>
Alarmingly, it was found that such problems occur even among previously healthy individuals and those who have had mild COVID-19 infections, according to the study findings.
Senior author, Dr Ziyad Al-Aly, MD, an assistant professor of medicine at Washington University told Thailand
Medical News, “Our study team wanted to build upon our past research on COVID's long-term effects by taking a closer look at what's happening in people's hearts.
What we're seeing isn't good. COVID-19 can lead to serious cardiovascular complications and death. The heart does not regenerate or easily mend after heart damage. These are diseases that will affect individuals for a lifetime."
To date almost 398 million people globally have been infected with the SARS-CoV-2 virus according to official data, but in reality, the actual figures could be four to five-fold!
Dr Al-Aly, who treats patients within the VA St. Louis Health Care System stressed,
"Consequently, COVID-19 infections have, thus far, contributed to 15 million new cases of heart disease worldwide. This is quite significant. For anyone who has had an infection, it is essential that heart health be an integral part of post-acute COVID care."
It was also reported that excess death rates globally due to heart failure is increasing phenomenally but governments and health authorities around the world are trying to downplay or conceal this emerging data and also conceal any correlation with exposure to the spike proteins of the virus and heart issues and fatalities arising as a result!
Cardiovascular disease is an umbrella term that refers to various heart conditions, thrombosis and stroke and is the leading cause of death in the United States and the world.
The Centers for Disease Control and Prevention (CDC) currently estimates that one out of every four deaths in America each year is due to heart disease.
https://www.cdc.gov/heartdisease/facts.htm#:~:text=
In 2020, roughly 659,000 Americans died from heart failure, and about 805,000 Americans had a heart attack.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000000950
It was estimated that the figures for 2021 which have yet to be published could be as high as 1.7 times!
Heart disease comes with a hefty price tag, according to the U.S CDC, costing the United States about US $363 billion each year in health-care services, medications and productivity lost to death.
Dr Al-Aly, who is also director of the Clinical Epidemiology Center and chief of the Research and Education Service at the Veterans Affairs St. Louis Health Care System added,
"For individuals who were clearly at risk for a heart condition before becoming infected with SARS-CoV-2, the findings suggest that COVID-19 may amplify the risk."
He further warned,
"But most remarkably, individuals who have never had any heart problems and were considered low risk are also developing heart problems after COVID-19. Shockingly our data showed an increased risk of heart damage for young people and old people; males and females; Blacks, whites and all races; people with obesity and people without; people with diabetes and those without; people with prior heart disease and no prior heart disease; people with mild COVID infections and those with more severe COVID who needed to be hospitalized for it."
The study team analyzed de-identified medical records in a database maintained by the U.S. Department of Veterans Affairs, the nation's largest integrated health-care delivery system.
The study team also created a controlled dataset that included health information of 153,760 people who had tested positive for COVID-19 sometime from March 1, 2020, through Jan. 15, 2021, and who had survived the first 30 days of the disease. Very few of the people in the study were vaccinated prior to developing COVID-19, as vaccines were not yet widely available at the time of enrollment.
Detailed statistical modeling was used to compare cardiovascular outcomes in the COVID-19 dataset with two other groups of people not infected with the virus: a control group of more than 5.6 million patients who did not have COVID-19 during the same time frame; and a control group of more than 5.8 million people who were patients from March 2018 through January 2019, well before the virus spread and the pandemic settled in.
The research does not include data involving the virus's delta and omicron variants, which began spreading rapidly in the latter half of 2021.
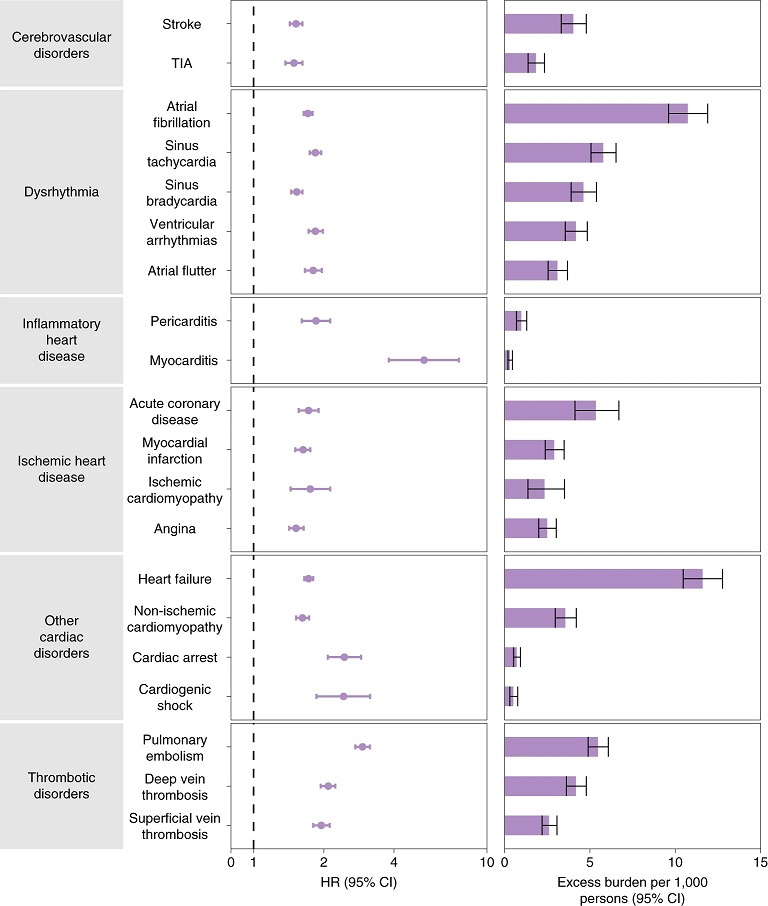 Risks and 12-month burdens of incident post-acute COVID-19 cardiovascular outcomes compared with the contemporary control cohort.
Outcomes were ascertained 30 d after the COVID-19-positive test until the end of follow-up. COVID-19 cohort (n = 153,760) and contemporary control cohort (n = 5,637,647). Adjusted HRs and 95% CIs are presented. The length of the bar represents the excess burden per 1,000 persons at 12 months, and associated 95% CIs are also shown.
Risks and 12-month burdens of incident post-acute COVID-19 cardiovascular outcomes compared with the contemporary control cohort.
Outcomes were ascertained 30 d after the COVID-19-positive test until the end of follow-up. COVID-19 cohort (n = 153,760) and contemporary control cohort (n = 5,637,647). Adjusted HRs and 95% CIs are presented. The length of the bar represents the excess burden per 1,000 persons at 12 months, and associated 95% CIs are also shown.
It should also be noted that the COVID-19 patients in the study were mostly older, white men; however, the study team also analyzed data that included women and adults of all ages and races.
The study team analyzed heart health over a year-long period. Heart disease, including heart failure and death, occurred in 4% more people than those who had not been infected with COVID-19.
Dr Al-Aly stressed, "Some people may think 4% is a small number, but it's not, given the magnitude of the pandemic. That translates to roughly 3 million people in the U.S. alone who have suffered cardiovascular complications due to COVID-19!"
Alarmingly when compared with those in the control groups without any SARS-CoV-2 infections, individuals who contracted COVID-19 were 72% more likely to suffer from coronary artery disease, 63% more likely to have a heart attack and 52% more likely to experience a stroke.
According to the study findings, overall, those infected with the SARS-CoV-2 virus were 55% more likely than those without COVID-19 to suffer a major adverse cardiovascular event, which includes heart attack, stroke and death.
Dr Al-Aly said, "The study findings highlight the serious long-term cardiovascular consequences of having a COVID-19 infection and emphasize the importance of getting vaccinated against COVID-19 as a way to prevent heart damage; this also underscores the importance of increasing accessibility to the vaccines in countries with limited resources."
He further added, "Governments and health systems around the world should be prepared to deal with the likely significant contribution of the COVID-19 pandemic to a rise in the burden of cardiovascular diseases. Because of the chronic nature of these conditions, they will likely have long-lasting consequences for patients and health systems, and also have broad implications on economic productivity and life expectancy. Addressing the challenges posed by long-COVID will require a much needed, but so far lacking, urgent and coordinated long-term global response strategy."
PERSISTENT CARDIAC INJURY IS COMMON AMONG COVID-19 SURVIVORS.
In the second study by researchers from Albert Einstein College of Medicine and Montefiore Medical Center-New York,-USA and Stony Brook University-New York, it was found that a high percentage of COVID-19 survivors who were hospitalized still had acute cardiac injury upon discharge and that persistent cardiac injury was common among COVID-19 survivors 2.5 months post-discharge.
Though acute cardiac injury (ACI) is a known COVID-19 complication, whether ACI acquired during COVID-19 recovery is unknown.
The study team investigated the incidence of persistent ACI and identified clinical predictors of ACI recovery in hospitalized patients with COVID-19 2.5 months post-discharge.
The retrospective study consisted of 10,696 hospitalized COVID-19 patients from March 11, 2020 to June 3, 2021. Demographics, comorbidities, and laboratory tests were collected at ACI onset, hospital discharge, and 2.5 months post-discharge. ACI was defined as serum troponin-T (TNT) level >99th-percentile upper reference limit (0.014ng/mL) during hospitalization, and recovery was defined as TNT below this threshold 2.5 months post-discharge. Four models were used to predict ACI recovery status.
The study findings shockingly showed that there were 4,248 (39.7%) COVID-19 patients with ACI, with most (93%) developed ACI on or within a day after admission.
In-hospital mortality odds ratio of ACI patients was 4.45 [95%CI: 3.92, 5.05, p<0.001] compared to non-ACI patients.
Of the 2,880 ACI survivors, 1,114 (38.7%) returned to our hospitals 2.5 months on average post-discharge, of which only 302 (44.9%) out of 673 patients recovered from ACI.
There were no significant differences in demographics, race, ethnicity, major commodities, and length of hospital stay between groups.
Prediction of ACI recovery post-discharge using the top predictors (troponin, creatinine, lymphocyte, sodium, lactate dehydrogenase, lymphocytes and hematocrit) at discharge yielded 63.73%-75.73% accuracy.
The study fining conformed that persistent cardiac injury is common among COVID-19 survivors. Readily available patient data accurately predict ACI recovery post-discharge. Early identification of at-risk patients could help prevent long-term cardiovascular complications.
The study findings were published in the peer reviewed journal: eBioMedicine by Lancet.
https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(22)00010-X/fulltext
The study team concluded, “
ACI is a common complication among hospitalized COVID-19 patients and many survivors exhibit persistent cardiac injury. Predictive models using a few readily available laboratory variables accurately predict ACI recovery status at 2.5 months post COVID-19. Our study has potential clinical implications because it suggests that ACI is an important marker of future adverse outcomes in COVID-19 and heightened awareness for cardiovascular complications is warranted when ACI is detected as cardiovascular prevention may have a lower priority in the context of treating SARS-CoV-2 infection. The ability to identify patients at-risk of persistent ACI early on would enable appropriate follow-up care to prevent long-term cardiac damage and other cardiovascular complications.”
Cardiovascular complications, cardiac injury and heart failures are expected to rise even more with the fast spreading Omicron variant that might present mild or asymptomatic conditions to a large majority initially but will consequently affect the heart in a variety of ways. Excess death rates due to heart failures are also expected to rise exponentially in coming months.
For more on
COVID-Cardiovascular Issues, keep on logging to Thailand Medical News.

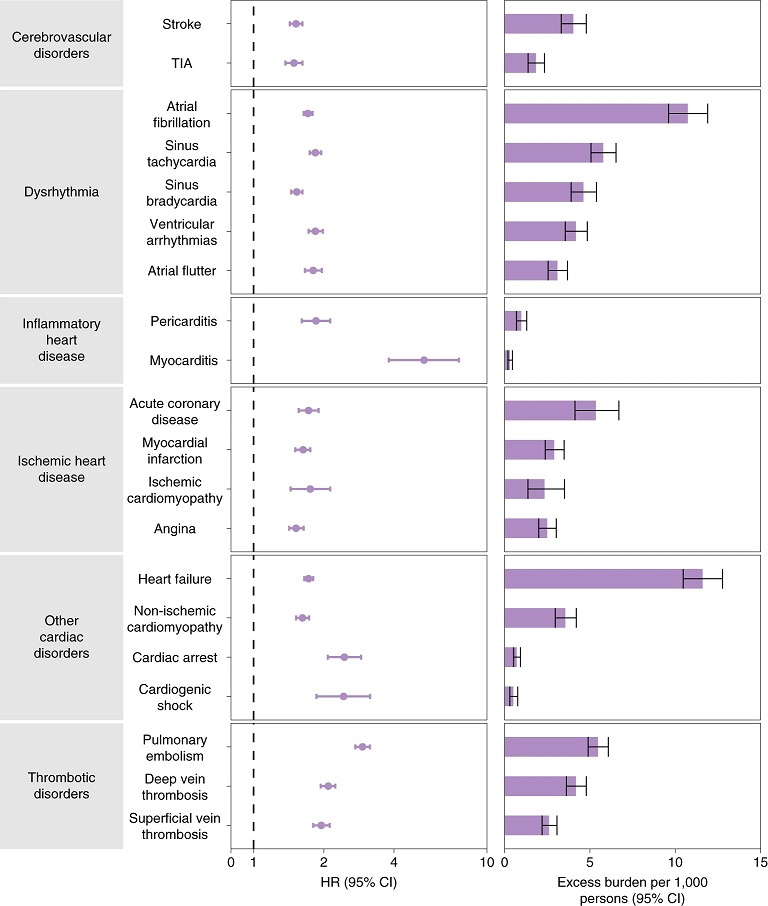 Risks and 12-month burdens of incident post-acute COVID-19 cardiovascular outcomes compared with the contemporary control cohort.
Risks and 12-month burdens of incident post-acute COVID-19 cardiovascular outcomes compared with the contemporary control cohort.